Abstract
Background
Repeated-sprint training (RST) involves maximal-effort, short-duration sprints (≤ 10 s) interspersed with brief recovery periods (≤ 60 s). Knowledge about the acute demands of RST and the influence of programming variables has implications for training prescription.
Objectives
To investigate the physiological, neuromuscular, perceptual and performance demands of RST, while also examining the moderating effects of programming variables (sprint modality, number of repetitions per set, sprint repetition distance, inter-repetition rest modality and inter-repetition rest duration) on these outcomes.
Methods
The databases Pubmed, SPORTDiscus, MEDLINE and Scopus were searched for original research articles investigating overground running RST in team sport athletes ≥ 16 years. Eligible data were analysed using multi-level mixed effects meta-analysis, with meta-regression performed on outcomes with ~ 50 samples (10 per moderator) to examine the influence of programming factors. Effects were evaluated based on coverage of their confidence (compatibility) limits (CL) against elected thresholds of practical importance.
Results
From 908 data samples nested within 176 studies eligible for meta-analysis, the pooled effects (± 90% CL) of RST were as follows: average heart rate (HRavg) of 163 ± 9 bpm, peak heart rate (HRpeak) of 182 ± 3 bpm, average oxygen consumption of 42.4 ± 10.1 mL·kg−1·min−1, end-set blood lactate concentration (B[La]) of 10.7 ± 0.6 mmol·L−1, deciMax session ratings of perceived exertion (sRPE) of 6.5 ± 0.5 au, average sprint time (Savg) of 5.57 ± 0.26 s, best sprint time (Sbest) of 5.52 ± 0.27 s and percentage sprint decrement (Sdec) of 5.0 ± 0.3%. When compared with a reference protocol of 6 × 30 m straight-line sprints with 20 s passive inter-repetition rest, shuttle-based sprints were associated with a substantial increase in repetition time (Savg: 1.42 ± 0.11 s, Sbest: 1.55 ± 0.13 s), whereas the effect on sRPE was trivial (0.6 ± 0.9 au). Performing two more repetitions per set had a trivial effect on HRpeak (0.8 ± 1.0 bpm), B[La] (0.3 ± 0.2 mmol·L−1), sRPE (0.2 ± 0.2 au), Savg (0.01 ± 0.03) and Sdec (0.4; ± 0.2%). Sprinting 10 m further per repetition was associated with a substantial increase in B[La] (2.7; ± 0.7 mmol·L−1) and Sdec (1.7 ± 0.4%), whereas the effect on sRPE was trivial (0.7 ± 0.6). Resting for 10 s longer between repetitions was associated with a substantial reduction in B[La] (−1.1 ± 0.5 mmol·L−1), Savg (−0.09 ± 0.06 s) and Sdec (−1.4 ± 0.4%), while the effects on HRpeak (−0.7 ± 1.8 bpm) and sRPE (−0.5 ± 0.5 au) were trivial. All other moderating effects were compatible with both trivial and substantial effects [i.e. equal coverage of the confidence interval (CI) across a trivial and a substantial region in only one direction], or inconclusive (i.e. the CI spanned across substantial and trivial regions in both positive and negative directions).
Conclusions
The physiological, neuromuscular, perceptual and performance demands of RST are substantial, with some of these outcomes moderated by the manipulation of programming variables. To amplify physiological demands and performance decrement, longer sprint distances (> 30 m) and shorter, inter-repetition rest (≤ 20 s) are recommended. Alternatively, to mitigate fatigue and enhance acute sprint performance, shorter sprint distances (e.g. 15–25 m) with longer, passive inter-repetition rest (≥ 30 s) are recommended.
Similar content being viewed by others
The most common RST set configuration is 6 × 30 m straight-line sprints with 20 s of passive inter-repetition rest. |
The reference estimates for HRavg (90% HRmax), VO2avg (~ 70–80% VO2max) and B[La] (10.8 mmol·L−1) demonstrate the substantial physiological demands of RST in team sport athletes. Associated prediction intervals for these estimates suggest that most of these demands are consistently substantial across many RST protocols, sports and athlete characteristics. |
Shorter inter-repetition rest periods (≤ 20 s) and longer repetition distances (> 30 m) amplify physiological demands and cause greater inter-set reductions in sprint performance (i.e. performance fatigue). Inversely, longer inter-repetition rest periods (≥ 30 s) and shorter repetition distances (≤ 20 m) enhance acute sprint performance and reduce the physiological demands. |
Shuttle-based protocols are associated with slower repetition times, likely due to the added change-of-direction component, but may reduce sprint decrement. The effect of shuttle versus straight-line RST protocols on physiological and perceptual outcomes remains inconclusive. |
Performing two less repetitions per set (e.g. four as opposed to six repetitions) maintains the perceptual, performance and physiological demands of RST. |
The findings from our investigation provide practitioners with the expected demands of RST and can be used to help optimise training prescription through the manipulation of programming variables. |
1 Introduction
Repeated-sprint training (RST) involves maximal-effort, short-duration sprints (≤ 10 s), interspersed with brief (≤ 60 s) recovery times [1]. It appears an effective and time-efficient training modality for physical adaptations in team-sport athletes, with as few as six sessions over two weeks shown to enhance high-speed running abilities [2]. The implementation of RST can also provide athletes with exposure to maximal sprinting, acceleration and deceleration, which are important components of team sport [3,4,5]. Throughout an athlete’s training program, there is a range of opportunities for RST to be used, such as during a pre-season where a progressive reduction in running volume and an increase in intensity is often implemented [6]. Alternatively, it could be employed during the playing season to promote the maintenance of specific physical qualities (e.g. speed, aerobic fitness), used as part of late-stage rehabilitation or implemented at a time when a training ‘shock-cycle’ is required. However, each training program requires different outcomes, with these attained through the manipulation of programming variables.
The type of stimulus is an important driver of the chronic adaptive response to training [7]. Repeated-sprint training is low-volume and short in duration, typically lasting 10–20 min per session, but due to the maximal intensity at which it is performed, it can generate adaptive events that ultimately result in the capacity for enhanced performance [8, 9]. This includes an improved aerobic and metabolic capacity [10,11,12,13,14,15,16,17]. However, there is considerable variation in RST prescription, with acute programming variables (e.g. sprint distance, rest duration, number of repetitions) regularly manipulated in research and practice [8, 18]. These changes can influence the internal and external load experienced by athletes during RST (i.e. the acute demands) and subsequently have the potential to cause diverse training adaptations [12]. For instance, in a study by Iaia et al. [19], higher within-set blood lactate concentration (~ 3 mmol⋅L−1 B[La]) was recorded during RST with shorter rest times (15 s versus 30 s), which can indicate a greater anaerobic contribution to exercise [20]. Accordingly, after six-weeks of training, the 15 s rest group achieved greater improvement in 200 m sprint time and the Yo-Yo intermittent recovery test level 2 compared with the 30 s group [19], with anaerobic energy production central to performance in these events [21, 22]. Thus, it is important to understand how the manipulation of programming variables affects the acute demands of RST, as this evidence can be useful to help explain how and why training adaptations may manifest.
There is conflicting evidence within and across studies regarding the effects of programming variables on the acute demands of RST. In a study by Alemdaroğlu et al. [23], B[La] and percentage sprint decrement (Sdec) were greater with 6 × 40 m shuttle repeated-sprints compared with the same straight-line protocol. Conversely, compared with shuttle-based sprints, straight-line sprints induced greater demands when more repetitions were performed over a shorter distance (8 × 30 m repeated-sprints) [23]. The prescription of active inter-repetition rest has been shown to promote higher heart rate and oxygen consumption (VO2) compared with passive rest [24]. However, Keir et al. [25] found that demands were greater when passive rest, fewer repetitions, shorter rest time and a longer sprint distance were prescribed. Ultimately, there is an infinite combination of programming variables that can alter the training outcome, but the acute effects of these factors are not well understood. Therefore, to guide training prescription and enhance the effectiveness of RST, it is important to gain a quantitative understanding of the acute effects of each programming factor.
While excessive training loads can contribute to fatigue, an appropriate training dose may allow for greater improvements in fitness and performance [26]. Knowledge of the acute demands of RST can help practitioners manage fatigue and target specific training outcomes. Therefore, our systematic review and meta-analysis aims to (1) identify the most common RST set configuration, (2) evaluate and summarise the acute physiological, neuromuscular, perceptual and performance demands of RST, and (3) examine the meta-analytic effects of sprint modality, number of repetitions per set, sprint repetition distance, inter-repetition rest modality and inter-repetition rest duration on the acute RST demands.
2 Methods
2.1 Search Strategy
This study was conducted in accordance with the ‘Preferred Reporting Items for Systematic Reviews and Meta-analyses’ (PRISMA) guidelines [27] and registered on Open Science Framework (Registration https://doi.org/10.17605/OSF.IO/2XQ3A). A systematic search of the literature was conducted to find original research articles investigating the acute demands of RST in team sport athletes. The latest search was performed on 10 January 2022, using the electronic databases Pubmed, SPORTDiscus, MEDLINE and Scopus. No restrictions were imposed on the publication date. Relevant keywords for each search term were identified through pilot searching of titles/abstracts/full-texts of previously known articles. Key search terms were grouped and searched within the article title, abstract and keywords using the search phrase (‘repeat* sprint*’ OR ‘intermittent sprint*’ OR ‘multiple sprint*’) AND (‘exercise’ OR ‘ability’ OR ‘training’) AND (‘team sport’ OR ‘players’ OR ‘athletes’) AND (‘physiological’ OR ‘perceptual’ OR ‘neuromuscular’ OR ‘metabolic’ OR ‘fatigue’) NOT (‘cycling’ OR ‘swimming’). No medical subject headings were applied to the search phrase.
Following the initial search of the literature, results were exported to EndNote library (Endnote X9, Clarivate Analytics, USA) and duplicates were removed. The remaining articles were then uploaded to Covidence (http://www.covidence.org, Melbourne, Australia), with the titles and abstracts independently screened by two authors (F.T., M.M.). Full-texts of the remaining articles were then accessed to determine their final inclusion–exclusion status. Articles selected for inclusion were agreed upon by both authors, with any disagreements resolved by discussion or a third author (J.W.). Furthermore, Google Scholar, as well as reference lists of all eligible articles and reviews [1, 8, 9, 28], were searched to retrieve any additional studies. Figure 1 displays the strategy for the study selection process used in this review.
2.2 Inclusion–Exclusion Criteria
The inclusion and exclusion criteria can be found in Table 1. We chose to omit any studies in which the mean athlete age was ≤ 16 years, as children may respond differently to RST [29, 30]. Studies were excluded if RST was performed in ≥ 30 °C because larger performance decrements may occur in hot compared with cool conditions [31]. We acknowledge that the residual effects of intense exercise may last up to 72 h [32], but acute demands measured up to 24 h following RST was selected because: (a) it is common for RST and other team sport activity to be interspersed with minimal recovery time (i.e. < 72 h), (b) pilot scoping of the literature only identified five studies [33,34,35,36,37] that recorded measurements on athletes > 24 h. Several studies/protocols were excluded from this investigation that implemented repeated-sprint sequences with sport skill elements [38,39,40,41,42] or involved a reactive component in response to an external stimulus (e.g. light sensor) [43,44,45,46]. Evidence from studies involving both single-set and multi-set repeated sprints was recorded, including the acute demands from repeated-sprint ability tests. For studies that involved pre-post testing of RST, separated by an intervention period (e.g. training, supplementation), only the RST baseline results were reported to ensure that the intervention period did not bias the results. Where observational time-series studies measured RST across a season, results were included for each phase (e.g. pre-season, mid-season, post-season), providing that no intervention was implemented outside of usual practice.
2.3 Classification of Study Design
To provide information on study design (Supplementary Table S2), studies were categorised under four designs as follows: (1) observational – non-experimental, (2) single group pre-test post-test – experimental treatment applied to a single group of participants, with the dependent variable/s measured before and after treatment, (3) crossover – two or more experimental conditions applied to the same participants, with or without a control condition, (4) parallel groups – two or more experimental conditions applied to two groups of different participants, with or without a control condition. Additionally, single-group time-series designs were categorised under observational and denoted.
2.4 Selection of Outcome Measures and Programming Variables
The outcome measures (Table 2) were selected on the basis of pilot scoping of the literature that identified commonly used indicators of internal responses to exercise and performance capacity in team sport settings [28, 47, 48]. Percentage sprint decrement, as defined by Fitzsimons et al. [49] and Glaister et al. [50], was chosen as it is the most ecologically valid index to quantify fatigue during RST [50]. However, caution should be taken when interpreting Sdec as weak relative and absolute reliability exists between repeated-sprint ability tests [51]. Blood lactate is sensitive to changes in exercise intensity and duration and is one of the preferred methods used to assess the anaerobic glycolytic contribution to exercise [20]. Sprint force–velocity–power parameters, as defined by Samozino et al. [52], and spring-mass model parameters, as defined by Morin et al. [53], were chosen as they represent field-based methods used to assess the mechanical effectiveness of sprinting and the neuromuscular manifestation of fatigue during over-ground running [54].
Programming variables recorded were: sprint modality (i.e. straight-line, 180° shuttle or multi-directional), number of repetitions per set, number of sets per session, sprint distance or duration per repetition, inter-repetition rest duration, inter-repetition rest modality, inter-set rest duration and inter-set rest modality.
2.5 Extraction of Study Information
Mean and standard deviation data were extracted directly from tables and within the text of the included studies. To obtain data from studies where information was provided in figures, graph digitising software (WebPlotDigitizer, version 4.3, USA) was used. For studies where rest duration was given as an exercise to rest ratio or on a time cycle that included sprint time, an estimated ‘actual’ rest time was also established. This was determined by extracting average sprint time (Savg) data from studies, where provided. For example, if Savg was 3.2 s and the recovery duration was given as 1:5 exercise to rest ratio, then the estimated recovery duration was 16 s, or if the recovery duration was given on a 30 s cycle, then the estimated recovery duration was 27 s, with recovery durations rounded to the nearest whole number.
With regards to sprint modality, shuttle repeated-sprints were defined as RST where one or more 180° changes of direction were performed. Multi-directional repeated-sprints involved RST where changes of direction were performed with angles other than 180°, but due to the large variety of designs (e.g. different angles and courses), this format was excluded from the meta-analysis. For rest modality, ‘passive’ included protocols where participants were required to walk back to a two-way start line (sprints alternating from both ends) in preparation for the next sprint. Where information relating to exercise protocols (e.g. sprint distance) could not be found within the study or clarification was required, authors were contacted. If authors did not respond, samples were removed from the meta-analysis. The Participant Classification Framework [55] was used to define training and performance calibre of the athletes included in our investigation (Supplementary Table S2).
Twenty-four estimates nested within 13 studies collected session ratings of perceived exertion (sRPE) via Borg’s 6–20 scale. For consistency with other included studies and to comply with more standard practice, 6–20 values were converted to Category–Ratio 10 (CR10®) units (deciMax) using the appropriate table conversion [56]. Standard deviations were converted by a factor that was proportionate to the mean value of each estimate, which ranged between 13–19 (conversion factors = 0.27–0.53). Where VO2 was expressed in absolute terms (L·min−1) [25], it was converted to relative terms (mL⋅min−1⋅kg−1) by extracting the mean body mass of the participants from the study. Where Sdec of 5% was set as the termination criteria [57], the mean number of repetitions was used for meta-analysis. Heart rates were inclusive of both the sprint component and inter-repetition rest periods, but samples were excluded [58] which continuously recorded heart rate during the inter-set rest periods. Due to a lack of studies reporting the effect of RST on peak heart rate (HRpeak) as a percentage of maximal heart rate (HRmax), this data was unable to be meta-analysed. However, these results [2, 59,60,61,62] are summarised in section 3.4.3. Post-exercise B[La] samples were meta-analysed together, irrespective of the exact time point that they were measured (i.e. 0–10 min). Although, for context, specific timepoints of each sample are given in Supplementary Table S3. Where studies provided multiple timepoints of B[La] collection, the highest value was used for meta-analysis. The considerable variation in measurement error between different jump systems makes it difficult to compare counter-movement jump (CMJ) height between different studies [63] and as such, CMJ height results were recorded, but not meta-analysed. For context, the type of jump measurement systems used in each study are noted alongside the results in Supplementary Table S3.
2.6 Assessment of Reporting Quality and Risk of Bias
To assess the reporting quality and risk of bias within the studies included in this review, two authors (F.T. and M.M.) independently evaluated the literature using a modified version of the Downs and Black index. This scale includes 14 original items and ranks each item as 0 or 1, with higher total scores (out of 14) indicating higher quality studies. The original Downs and Black scale was reported to have acceptable test–retest (r = 0.88) and inter-rater reliability (r = 0.75) [64]. If there was an absence of clear information to assess an item on either scale, it was scored as 0. Any disagreements between the two authors were resolved by discussion or a third author (J.W.).
2.7 Data Analysis
All analyses were performed in the statistical computing software R (Version 4.0.0; R Core Team, 2020). Studies eligible for meta-analysis often reported RST outcomes from several subgroups (e.g. elite versus non-elite, males versus females, etc.), from repeated measures taken on the same group of athletes (e.g. set 1 and set 2, warm-up A versus warm-up B, etc.), or a combination of both. To appropriately account for this hierarchical structure, in particular, the within-study correlation arising from repeated measures [65] and on the assumption that the true acute demand of RST varies between studies [66], data were analysed using multi-level mixed-effects meta-analysis via the metafor package [67]. Initial (baseline) models were run for each outcome measure with 10 or more estimates and fit using restricted maximum-likelihood. These models included only random effects, which were specified in a nested structure as studies (i.e. individual research papers; outer factor) and groups within studies (inner factor, [65]). Units of analysis were therefore individual estimates from groups within studies, given as the mean value of the outcome measure following RST. Both the associated standard deviation (SD) and sample size were used to calculate the variance of each estimate. When a study involved repeated measures (i.e. multiple rows of data for the same group of athletes), dependency was accounted for by replacing variance with the entire ‘V’ matrix; that is, the variance–covariance matrix of the estimates [65]. Block-diagonal covariance matrices were estimated with an assumed correlation of r = 0.5 using the clubSandwich package [68]. Since it is uncommon for studies to report the correlation coefficient between repeated measures [69], our assumption was informed by re-analysis of our previous (unpublished) work in team-sport RST.
Uncertainty in meta-analysed estimates was expressed using 90% compatibility (confidence) intervals (CI), calculated based on a t-distribution with denominator degrees of freedom given from the unique number of ‘group’ levels (i.e. the inner level of the random effects structure). Pooled estimates were also presented with 90% prediction intervals, which convey the likely range of the true demand of RST in similar future studies [70]. Between-study and between-group heterogeneity in each meta-analysed estimate was quantified as a SD [Sigma (σ)] [71]), with 90% CI calculated using the Q-profile method [72].
To examine the effect of programming variables on acute RST outcomes, candidate factors were added to the aforementioned baseline models as fixed effects for outcomes with sufficient estimates available (approximately 10 per moderator [73]). The five moderator variables were: sprint modality (categorical: straight-line or 180° shuttle), number of repetitions per set (continuous, linear), total distance covered in each repetition (continuous, linear), inter-repetition rest modality (categorical: active or passive) and inter-repetition rest duration (continuous, linear). Factors were re-scaled so that the reference (intercept) effect represented the performance or response to 6 m × 30 m straight-line sprints with 20 s passive rest between repetitions. The effects of each moderator were then estimated (along with 90% CI and 90% prediction intervals, where appropriate), with all other factors being held constant. Categorical moderators were given as the difference between levels (shuttle compared with straight-line sprints and active compared with passive inter-repetition rest). Continuous moderators were evaluated at a magnitude deemed to be practically relevant for training prescription: performing two more repetitions, sprinting 10 m further per repetition and resting for 10 s longer between repetitions. The effects of repetition distance on repetition time (average and fastest sprint) were not shown (but were still offset to a distance of 30 m), because the time taken to complete a sprint repetition is almost entirely dependent on the distance to be covered. The total amount of variance explained by the combination of moderators was given as a pseudo-R2 value, calculated by subtracting the total (pooled) variance from final models (\(\sigma_{{{\text{mods}}}}^{2}\)) as a fraction of baseline models (\(\sigma_{{{\text{base}}}}^{2}\)) from 1 (1 − \([\sigma_{{{\text{mods}}}}^{2} /\sigma_{{{\text{base}}}}^{2} ]\)).
To provide an interpretation of programming moderators, we (subjectively) considered the entire range of the CI representative of values compatible with our models and assumptions [74], relying mostly on the point estimate. To further contextualise the practical relevance of moderators, we visually scaled effects against regions of practical significance. That is, reference values for each outcome measure that have been empirically or theoretically anchored to some real-world importance in the context of team-sport athletes and/or RST. These thresholds were: 2 bpm (~ 1%) in HRpeak [75], 1 au in CR10-scaled sRPE [76], a 1% faster or slower sprint time [77] based on the reference performance given as the intercept: 0.05 s for Savg, 0.04 s for best sprint time (Sbest) and 1% for Sdec across a set [77]. In absence of a recognised practical reference value for a change in B[La] above the anaerobic threshold, we used the value of a small, standardized effect. Between-athlete standard deviations from included estimates (n = 120) were meta-analysed on the log scale, as previously described (SD = 1.9 mmol·L−1, 90% CI 1.7–2.22), before being multiplied by 0.2. The threshold for a moderate standardised effect (0.6 × 1.9 mmol·L−1) was also calculated and shown for visual purposes. When a CI fell entirely inside the region of practical significance or predominantly inside one region, we declared an effect as trivial. When a CI fell entirely outside the region of practical significance or predominantly outside the region, we declared an effect substantial. If there was equal coverage of the CI across the trivial region and the substantial region in only one direction (i.e. positive or negative), the effect was deemed compatible with both trivial and substantial effects. Finally, when the CI spanned across substantial regions in both positive and negative directions, including the trivial region, an effect was deemed inconclusive.
3 Results
Following the screening process (Fig. 1), 215 publications were included in our investigation, with data from 908 samples nested within 176 studies eligible for meta-analysis. Across all studies, there were 4818 athlete inclusions from 282 repeated-sprint protocols reported.
3.1 Study Characteristics
The most common study design for investigations of acute demands of RST was single group, cross sectional observational (n = 87 studies, 40%). Soccer was the most investigated sport (n = 104, 48%), followed by basketball (n = 33, 15%), rugby (league, union and sevens) (n = 15, 7%), futsal (n = 14, 7%), handball (n = 12, 6%), field hockey (n = 10, 5%), Australian rules football (n = 5, 2%), volleyball (n = 3, 1%), netball (n = 2, 1%) and a mixture of team sports (n = 17, 8%). Of these sports, 21 (10%) studies involved elite/international level athletes, 125 (58%) studies involved highly trained/national level athletes and 58 (27%) studies involved trained/development level athletes, with 11 (5%) studies not reporting the training and performance calibre of the athletes. Female athletes were represented in 31 (14%) studies. A summary of the participants and study characteristics of included publications are provided in Supplementary Table S2.
3.2 Outcomes for the Assessment of Reporting Quality and Risk of Bias
Supplementary Table S1 summarises the outcomes of the modified Downs and Black scale for the assessment of reporting quality and risk of bias. Results ranged from 7 to 12, with a mean score of 9.6 ± 0.9.
3.3 Study Outcomes
A summary of the training protocols and study outcomes of included publications are provided in Supplementary Table S3.
Performance outcomes were represented in 198 (92%) of studies and the most common outcome measure was Sdec (n = 127 studies, 59%) (Fig. 2). The most common prescription of each programming variable were straight-line sprints (n = 153 protocols, 54%), performed over 30 m (n = 107, 38%), with a passive recovery (n = 186, 66%) lasting 20 s (n = 83, 29%), prescribed as one set of six repetitions (n = 122, 43%; Fig. 3). The majority of protocols (n = 263, 93%) employed one set of repeated-sprints, with two sets, three sets and four sets used in five (2%), ten (4%) and four (1%) protocols, respectively. The most common inter-set rest times for all multi-set protocols were 4 (six protocols) and 5 mins (five protocols). The number of 180° changes of direction prescribed for shuttle repeated-sprints ranged from one to two. The most prescribed mode of active recovery was a slow jog back to a one-way start line (n = 32 protocols, 33%, i.e. sprints start from one end only). There was one study [33] that strictly enforced a 5 m deceleration zone and one other study [78] that enforced a 6 m deceleration zone.
The distribution of outcome measures. Data given as the total number of studies represented (out of 215). Sbest best sprint time, Savg average sprint time, Stotal total sprint time, Sdec percentage sprint decrement, CMJ counter-movement jump, SMM spring-mass model characteristics, FVP sprint force–velocity–power profiling, sRPE ratings of perceived exertion, HR heart rate, B[La] blood lactate, CK serum creatine kinase, VO2 oxygen consumption
3.3.1 Meta-analysed Acute Demands of Repeated-Sprint Training
The acute physiological, perceptual and performance demands of RST in team sport athletes are presented in Table 3. Also presented are the 90% CI and PI for each estimate, as well as the between sample and between study variation (σ).
3.3.2 Moderating Effects of Programming Variables on the Acute Demands of Repeated-Sprint Training
The moderating effects of programming variables on the acute physiological, perceptual and performance demands of RST are presented in Figs. 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15. All effects were evaluated as the change in each outcome measure when compared with a reference protocol of 6 m × 30 m straight-line sprints with 20 s passive inter-repetition rest. Unless noted in the subsequent sections, moderating effects were deemed inconclusive [i.e. a confidence level (CL) spanning across substantial regions in both positive and negative directions, including the trivial region].
3.3.2.1 Shuttle-Based Sprints
Shuttle-based sprints were associated with a substantial increase in Savg and Sbest (i.e. slower times; Figs. 10, 11, 12, 13), whereas the effect on sRPE was trivial (Figs. 6, 7). Performing shuttle-based sprints was compatible with both a trivial and substantial reduction in Sdec [i.e. a less pronounced decline in sprint times (faster) throughout the set; Figs. 14 and 15].
3.3.2.2 Performing Two More Repetitions Per Set
Performing two more repetitions per set had a trivial effect on HRpeak (Figs. 4 and 5), sRPE (Figs. 6 and 7), Savg (Figs. 12 and 13), Sdec (Figs. 14 and 15) and B[La] (Figs. 8 and 9). Additionally, performing two more repetitions per set was compatible with both a trivial and substantial increase in Sbest (i.e. slower time; Figs. 10 and 11).
3.3.2.3 Sprinting 10 m Further Per Repetition
Sprinting 10 m further per repetition was associated with a substantial increase in B[La] (Figs. 6 and 7) and Sdec [i.e. a more pronounced decline in sprint times (slower) throughout the set; Figs. 14 and 15], whereas the effect on sRPE was trivial (Figs. 6 and 7). Additionally, sprinting 10 m further per repetition was compatible with both a trivial and substantial increase in HRpeak (Figs. 4 and 5). The effects on Sbest and Savg were not evaluated.
3.3.2.4 Resting for 10 s Longer
Resting for 10 s longer between repetitions was associated with a substantial reduction in B[La] (Figs. 8 and 9), Savg (Figs. 12 and 13), and Sdec (Figs. 14 and 15), while the effects on HRpeak (Figs. 4 and 5) and sRPE (Figs. 6 and 7) were trivial. Resting for 10 s longer between repetitions was compatible with both a trivial and substantial reduction in Sbest (i.e. faster time; Figs. 10 and 11).
3.3.2.5 Performing Active Inter-Repetition Rest
Using an active inter-repetition rest modality was compatible with both a trivial and substantial increase in HRpeak (Figs. 4 and 5), sRPE (Figs. 6 and 7) and Sdec (Figs. 14 and 15).
3.3.3 Acute Demands of Repeated-Sprint Training on Non-Meta-Analysed Outcomes
The acute demands of straight-line and shuttle RST on non-meta-analysed outcomes are as follows: total sprint time ranged from 7.82 to 86.09 s (number of studies = 102, number of samples = 185), end-set heart rate (HRpost) ranged from 139 to 191 bpm (n = 4 and 12), HRpeak as % HRmax ranged from 85% to 97% (n = 4 and 12), average VO2 as a percentage of maximal oxygen consumption (VO2max) ranged from 73% to 83% (n = 3 and 6) and creatine kinase measured 24 h post-session ranged from 354 to 1120 µ·L−1 (n = 6 and 8). The absolute change in CMJ height ranged from 2.4 to −8.6 cm (n = 9 and 20) and the percent change ranged from 8% to −27% (n = 10 and 21). Results from studies that investigated spring-mass model parameters (n = 2 and 2) and sprint force–velocity–power parameters (n = 1 and 1) are provided in Supplementary Table S3.
3.3.4 Acute Demands of Multi-directional Repeated-sprint Training
The acute demands of multi-directional RST are as follows: Sdec ranged from 1% to 7% (number of studies = 13, number of samples = 24), Sbest ranged from 4.36 to 8.21 s (n = 11 and 19), Savg ranged from 4.14 to 8.39 s (n = 12 and 22), total sprint time ranged from 32.22 to 83.99 s (n = 9 and 11), end-set B[La] ranged from 5.4 to 15.4 mmol·L−1 (n = 6 and 8), sRPE ranged from 5.5 to 9.1 au (n = 6 and 10) and HRpeak ranged from 178 to 195 b·min−1 (n = 6 and 10).
4 Discussion
This systematic review and meta-analysis provides the first comprehensive synthesis of the acute demands of RST in team sport athletes. It contains data from 215 studies, 282 repeated-sprint protocols and 4818 athlete inclusions. We demonstrate that physiological, neuromuscular, perceptual and performance demands incurred during RST are consistently substantial; a finding supported by both the meta-analysed point estimates and their 90% prediction intervals (Table 3). Moreover, the magnitude of these acute demands can be influenced by the manipulation of programming variables (Table 4). Prescribing longer sprint distances (> 30 m) and/or shorter (≤ 20 s) inter-repetition rest can increase physiological demands and performance decrement. Conversely, the most effective strategy to mitigate the acute decline in sprint performance is the prescription of longer inter-repetition rest times (≥ 30 s) and shorter sprint distances (15–25 m). The effects of performing two more repetitions per set on our outcomes was trivial, which suggests that prescribing a lower number of successive sprints (e.g. four as opposed to six) may be a useful strategy to reduce sprint volume, while maintaining the desired physiological demands. The influence of shuttle-based protocols and inter-repetition rest modality remain largely inconclusive. These findings from our review and meta-analysis can be used to inform RST prescription and progression in team sport athletes.
Repeated-sprint training is one method among an array of training options that practitioners can use to enhance the physical performance of team sport athletes. The meta-analytic estimate of sRPE (Table 3) indicates that RST is perceived to be ‘very hard’ (90% PI: ‘moderate’ to ‘extremely hard’), which agrees with the intended prescription of this training modality [18, 79]. Taking into account that a typical RST session lasts for between 10–20 min, the sRPE-training load (sRPE × training duration) is a fraction of that observed during team sport practice [80,81,82], being approximately 65–130 au (deciMax units). However, this should be considered alongside the physiological and neuromuscular stresses imposed by the RST session. The 10.1–11.3 mmol·L−1 reference estimate of B[La] is well above the second lactate threshold (~ 4 mmol·L−1) and therefore indicates that there is an immediate and intensive demand placed on the anaerobic glycolytic system during RST [83]. A high rate of anaerobic energy production, accompanied by a B[La] response exceeding 10 mmol·L−1, may be an important stimulus to elicit positive long-term changes in enzymes central for anaerobic glycolysis [28, 84]. Therefore, to potentially optimise the anaerobic adaptations to RST for team sport athletes, sessions that cause a B[La] demand of > 10 mmol·L−1 should be prescribed. Practitioners should also be conscious of the neuromuscular demands (i.e. impairment in the muscles ability to produce force) imposed by RST, with considerable decrements in CMJ height observed immediately after its implementation. However, while fatigue may be detrimental to acute performance, it also can be important for adaptation [85].
Athletes can reach VO2max during RST [86] and the average VO2 demand is considerable (Table 3), corresponding to approximately 70%–80% of VO2max for the normal team sport athlete [87,88,89,90]. This also agrees with studies reporting the average VO2 demands of RST as a percentage of the athletes measured VO2max [24, 59, 60]. Training sessions spent with longer periods of time at a high percentage of VO2max have been suggested to be an optimal stimulus for enhancing aerobic fitness, particularly in well-trained athletes [79, 91,92,93]. If the objective is to maximise aerobic adaptations, practitioners should therefore prescribe RST sessions that induce an average VO2 demand of > 90% max (or > 95% maximal heart rate) [79, 94], which could be achieved by manipulating certain programming variables in isolation and/or combination. Although moderator analysis of VO2 was not feasible due to a low number of samples, qualitative synthesis indicates that longer sprint distances [86], active rest periods [24] and shuttle-based RST [59, 60] can amplify the VO2 demands. While RST is a time-efficient training method that can induce small to large improvements across a range of physical parameters [8, 9], practitioners should, however, consider that RST is unlikely to be the best tool for eliciting time at or near VO2max and ultimately, for enhancing aerobic fitness [9, 79]. Pursuing utmost change in this area by implementing excessively demanding protocols could mitigate the improvement of other physical qualities (e.g. speed). Manipulating programming variables based on the goals of the training program is therefore crucial to regulate the acute demands of RST and optimise specific adaptations.
4.1 Sprint Modality
There were a greater number of RST protocols that prescribed straight-line sprints (n = 153, 54%) compared with shuttle RST (n = 105, 37%) and multi-directional RST (n = 24, 9%). Across the 24 protocols that prescribed multi-directional repeated-sprints [46, 95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111], there were a variety of different designs and angles implemented, ranging from 45° to 135°, for 2–5 changes of direction. Given the multitude of programming variables to consider, meta-analysis of multi-directional RST was not feasible. Nonetheless, we found that consistently high HRpeak (178–195 bpm and 92%–100% HRmax), sRPE (5.5–9.1 au) and post-session B[La] (5.4–15.4 mmol·L−1) were reported across all multi-directional protocols. Multi-directional sequences were designed to replicate specific movement demands of team sports, where rapid changes of direction are common [5, 112, 113]. Moreover, previous research has identified that straight-line speed and change of direction ability are different physical qualities because of their distinct biomechanical determinants [112, 113]. Greater application of multi-directional and shuttle-based RST may therefore be used to help develop change of direction ability, but practitioners should be aware of the acute demands of each modality.
Compared to straight-line RST, our meta-analysis shows that sprint times are clearly slower during shuttle-based RST (Figs. 10 and 12), but Sdec is less (Fig. 14). Practitioners can therefore expect slower sprint velocity when changes of direction are implemented, but athletes may be able to better sustain their initial sprint performance. The effects on HRpeak and B[La] were inconclusive (Figs. 4 and 8), while the effect on sRPE was mostly trivial (Fig. 6), which may suggest that these physiological and perceptual demands of RST are independent of sprint modality. It should be noted, however, that the acute demands of RST performed with changes of direction are conditional to the number and angle of direction changes, the distance between each direction change and the duration of the sequence [60, 99, 106, 114, 115]. These factors affect the absolute speeds that are attained and the muscular work performed during the sprint, propulsive and braking components. Additionally, by integrating changes of direction into RST, there is accumulation of acceleration and deceleration which can increase the neuromuscular demand [99]. This seems evident by greater reductions in CMJ height following shuttle-based RST [104, 116, 117].
Shuttle-based sprints can be applied during a RST program to emphasise change of direction, limit absolute running speeds and induce a similar physiological demand to straight-line RST. There may be instances, such as towards the end of season, where practitioners want to limit the physiological stress on the athlete during shuttle or multi-directional RST. In these cases, it has been demonstrated that decreasing the sprint duration through time-matched protocols is an effective strategy [99]. Therefore, when designing RST, practitioners need to consider the influence of the direction changes on the duration of the sprint, rather than just the overall distance, as this can have a marked effect on the internal demands [99]. Of course, straight-line sprints should be implemented if the goal is to expose athletes to higher speeds.
4.2 Number of Sprint Repetitions and Sets
Repeated-sprint training is implemented in research and practice to target a broad range of outcomes, which is reflected by considerable variation in the number of sprint repetitions prescribed across studies (range 2–40 repetitions per set). The vast majority of protocols (n = 257, 94%) implemented just one set, with six repetitions the most prescribed number of sprints per set (n = 122 protocols, 43%). Protocols that prescribed ≥ 12-repetitions per set [19, 33,34,35, 61, 62, 86, 118,119,120,121,122,123,124,125,126,127,128] were often designed to induce a high degree of fatigue. Accordingly, high creatine kinase responses (542–1127 µ·L−1) were reported in studies prescribing high repetition protocols [33,34,35, 123], despite longer inter-repetition rest times (≥ 30 s). These long-series of exhaustive efforts are counterintuitive to the movement demands of team sports, where sprint efforts are more likely to occur in small clusters [129, 130]. While the moderating effects of the number of sets per session was not meta-analysed due to the low number of samples, it is worth noting that with an increasing number of sets, sprint times decayed and heart rate was increased, but changes in B[La] seem negligible [58, 122, 131]. Further investigation is required to better understand the impact of the number of sets performed per session, as well as the overall session volume, on the acute demands of RST.
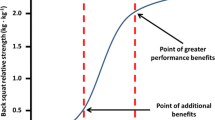
A substantial physiological demand is induced with the prescription of just six sprint repetitions, as demonstrated by the estimates and PI’s for HRpeak and B[La] (Figs. 4 and 8). A large cardiac demand, inferred by the 182 bpm reference estimate of HRpeak, coupled with a B[La] response exceeding 10 mmol·L−1, provide a strong aerobic and anaerobic stimulus, which may underpin the improvements in high-speed running abilities observed after RST interventions [2, 8]. With the reference estimate of B[La] above 10 mmol·L−1 and HRpeak close to maximal after six repetitions, further pursuing small increases in these acute physiological outcomes by performing more repetitions does not seem worthwhile. Our meta-analytic estimates show that the effects of performing two more repetitions per set was trivial on all outcome measures except Sbest, which was compatible with both trivial and substantial effects (Fig. 10). Therefore, other programming factors appear to have a greater effect on physiological, perceptual and performance outcomes. Crude estimation of the number of additional sprints required for the point estimate of each outcome measure to equal the minimum practically important difference reveals an unrealistic and impractical expectation. For example, the number of additional repetitions needed to increase sRPE by a one-unit scale change in our data is ten (i.e. 16-repetitions per set in total). This increase in volume and the neuromuscular demands of high repetition sets (greater than ten repetitions) may induce excessive muscle damage [33,34,35, 123]. Moreover, large numbers of repetitions can result in ‘pacing’ strategies that influence the maximal nature of RST and accumulated fatigue reduces the effectiveness of later sprints [132]. This is supported by our findings that show a Sdec of 1.2% would be expected to occur in studies (groups) performing 6 more repetitions (i.e. 12-repetitions per set in total) [77]. Therefore, excessive numbers of sprint repetitions can exacerbate fatigue and cause sub-optimal performance during RST.
Lower numbers of repetitions per set (e.g. greater than six repetitions) may be a more effective programming approach during competition periods to reduce training volume while still providing a potent physiological stimulus and allowing for the quality of each repetition to be maintained. In this regard, the trivial reduction expected in each outcome measure when performing four versus six repetitions may be beneficial, when viewing from a risk-reward perspective. However, a one-size-fits-all approach regarding the RST prescription for team sport athletes can lead to some athletes being under-stimulated, while others can be overloaded, depending on the athletes’ speed and fitness profile [133, 134]. When the number of repetitions performed is fixed, there is considerable inter-individual variation in the degree of fatigue experienced across the same group of athletes [48]. This can be incurred despite two athletes having similar maximal aerobic speeds but different maximal sprinting speeds (i.e. differences in anaerobic speed reserve) [134, 135]. In our review, all studies, except one [57], prescribed a fixed number of repetitions. However, in the study by Akenhead et al. [57] the level of relative sprint decrement (5%) was prescribed with a ‘flexible’ repetition scheme, which allowed more control over the magnitude of fatigue accrued by all participants. By prescribing a level of relative sprint decrement or relative performance threshold, instead of a fixed number of repetitions, practitioners can individualise RST prescription. This could provide practitioners with the ability to autoregulate training load based on differences in physical capacities and fluctuations in prior fatigue.
4.3 Sprint Distance
A sprint distance of 30 m was most implemented (n = 107 protocols, 38%), which is longer than the average sprint distance typically observed during field-based team-sports competitions (15–25 m) [136]. Additionally, 40 m was the longest sprint distance prescribed (n = 74, 26%). This distance is commonly used as a proxy measure of maximal speed in team sport athletes [137, 138], as it can allow maximal velocity to be reached when it is applied in a straight-line format. Furthermore, both 30 m and 40 m were often implemented as a shuttle format, with one to two changes of direction. A distance of 14 m was the shortest sprint effort prescribed, represented in two protocols [139], while 15 m was prescribed in 11 (4%) protocols. Compared with longer sprints (> 30 m), these shorter distances emphasise the acceleration phase of sprinting and were often applied with court-based athletes (i.e. basketball and handball) [122, 139,140,141]. Shorter distances may better reflect the competitive environment of court-based team sports where players are engaged in sprint efforts of 15 m and less [119, 142, 143].
Despite the prevalence of studies implementing a sprint distance of 30 m, altering the distance of each sprint effort by 10 m had the largest moderating effect on B[La] (substantial increase), Sdec (substantial increase [more pronounced decline in sprint times]) and HRpeak (compatible with a trivial and substantial increase). Longer sprints increase phosphocreatine (PCr) depletion and glycolytic activity, while also resulting in an increased accumulation of metabolic by-products (e.g. hydrogen ions, inorganic phosphate) [1, 136]. Furthermore, longer sprints provide exposure to faster absolute running speeds and higher vertical ground reaction forces that are attained via upright running mechanics [144, 145]. This is compared with shorter distances, where the athlete spends a high proportion of time in the acceleration phase, resulting in a greater horizontal propulsive force, but smaller braking force [144, 145]. Consequently, there can be a greater strain on the musculoskeletal system during longer sprints [146,147,148]. This is evident through greater declines in sprint kinematics (i.e. vertical stiffness and centre of mass vertical displacement) when longer sprint distance (35 m versus 20 m) was prescribed in two studies that investigated spring-mass model characteristics [54, 149]. Despite a greater physiological and neuromuscular demand imposed by longer sprints, the effect of a 10 m longer sprint on sRPE was trivial (Fig. 6). This suggests that greater distances can be prescribed without inducing a practically substantial increase in perceived exertion.
When beginning a RST program, shorter distances (15–25 m) are a more conservative option that can be used to limit metabolic stress and neuromuscular strain. It may also be beneficial to prescribe shorter distances during maintenance/taper sessions or for athletes who may never be exposed to longer sprints during competition (e.g. court-based athletes, goalkeepers). Training progression and overload can then be achieved by gradually increasing distance (> 30 m) with a view to expose athletes to faster absolute running speeds, greater fatigue and a high physiological demand. This could be implemented during preparation phases before commencing high-intensity training drills and match-play, or during late-stage return to play following injury.
4.4 Inter-repetition Rest Duration
There was considerable heterogeneity in the distribution of inter-repetition rest duration across the protocols, which ranged from 10 to 60 s. This was partly due to differences in the approach to rest prescription, whereby pre-determined times, time-cycles and work-to-rest ratios were all employed in different literature. A 10 s rest duration was prescribed in 11 (4%) protocols, but such short rest may make it difficult for athletes to safely decelerate and make it back to the start-line in time for the next sprint. The most common rest durations were 20 s and 30 s, represented in 83 (29%) and 67 (24%) protocols, respectively. These rest durations are similar to the amount of recovery time typically afforded between sprints during team sport competition [129, 130]. A 60 s rest duration was implemented in 9 (3%) protocols.
Shorter rest times (e.g. 10 s versus 20 s) are associated with slower sprint times, greater performance fatigue and an increased metabolic response. Additionally, shorter rest may lead to greater decrements in CMJ height following RST [150]. Inversely, longer inter-repetition rest times (e.g. 30 s vs 20 s) have a substantial influence on the reduction of B[La] and allow for sprint performance to be better maintained across a set (i.e. faster Savg and lower Sdec). This is likely due to greater clearance of metabolic by-products and increased PCr resynthesis [1, 121]. An interesting finding of our study was that a 10-s longer inter-repetition rest had a trivial effect on HRpeak and sRPE. Longer inter-repetition rest may allow athletes to perform each repetition with greater speed [151] and reduce the desire for pacing. Furthermore, longer rest would be expected to increase set duration, thereby allowing both heart rate and VO2 to increase with time [86, 106, 122]. It is possible, however, that the cardiorespiratory demand could be blunted if prolonged rest times (e.g. 60 s) are implemented. This was demonstrated in a group of well-trained university students where VO2 was 9% less when 60-s rest times were used during RST, compared with 30 s rest [151].
Collectively, our findings support the use of longer rest durations (≥ 30 s) to reduce within session fatigue and maintain repetition quality. Longer rest times could therefore be implemented during periods of fixture congestion to reduce player fatigue during RST, or used during the intensification stage of a pre-season to maximise sprint performance [19]. Additionally, longer rest times are recommended when longer sprint distances are prescribed, which can help account for the extended work duration of these sequences. However, longer rest durations reduce the metabolic demand of RST, which could limit certain physiological adaptations (e.g. maximal accumulated oxygen deficit, changes in glycolytic enzymes) [28, 152] and performance in activities that require a substantial anaerobic component [19]. Therefore, shorter rest durations (≤ 20 s) can be prescribed to induce greater levels of fatigue, which could help prepare team-sport athletes for peak periods of a match, where sprint efforts can be interspersed with minimal rest [129, 130].
4.5 Inter-repetition Rest Modality
There were a higher number of protocols that implemented passive inter-repetition rest (n = 186, 66%), as opposed to an active rest period (n = 96, 34%). Active recovery protocols were commonly combined with inter-repetition rest durations of ≥ 25 s. Most protocols that prescribed an active recovery involved a slow jog at pre-defined running speeds (e.g. 2 m⋅s−1) or self-selected speeds, which were often returning to a one-way start line. Other active recovery protocols implemented faster running speeds such as 8 km⋅h−1 [23, 118] and 50% of maximal aerobic speed [24, 86, 153, 154]. When these faster running speeds were prescribed, the physiological demands (i.e. heart rate, VO2, B[La]) were amplified and there was a greater Sdec compared with passive rest and active rest performed at a slow jog [24, 153,154,155]. Repeated jumps were performed during the inter-repetition rest period in two studies [59, 156], which increased the cardiorespiratory and muscular demands [59, 156]. However, the internal demands are likely to be more varied compared with a precise running intensity.
The findings of our meta-analysis suggest that active rest may cause a substantial increase in HRpeak (Fig. 4), sRPE (Fig. 6) and Sdec (Fig. 14), although we acknowledge that these effects are also compatible with trivial values (i.e. there could be no substantial influence). Active recovery limits the oxidative potential for PCr resynthesis before each sprint, which affects the maintenance of muscle power [24, 133, 150]. This leads to greater declines in anaerobic work capacity and subsequently, repeated-sprint performance. On the contrary, passive recovery is associated with an enhanced PCr resynthesis and as our results confirm, a smaller Sdec [157, 158]. While there were no substantial differences in B[La] (Fig. 8), our meta-analysis does not consider the intensity of the recovery period, which ultimately determines the extent of the acute demands [59, 153, 157].
The prescription of active recovery might amplify the physiological and perceptual demands to RST, as well as performance decrement, without increasing the sprint volume. This could be achieved, for example, by prescribing active recovery at an intensity of ≥ 50% maximal aerobic speed. It would be practical to implement this with a standardised recovery-run distance and rest durations of ≥ 25 s to allow the athlete to gradually decelerate from the sprint component into the recovery running speed. Yet, once again, acknowledging that the influence of active recovery on HRpeak, sRPE and Sdec were compatible with both trivial and substantial effects, we advise practitioners to place more emphasis on recovery duration for manipulating RST acute demands at present. For this reason, future research should examine the effects of specific active recovery intensities on RST physiological, perceptual, neuromuscular and performance demands.
4.6 RST Protocols with Additional Modifications
The use of additional modifications to RST can be applied to augment or attenuate internal demands. Short enforced deceleration zones (< 10 m), which were prescribed in two studies [33, 78], reduce sprint performance and exacerbate the magnitude of muscle damage due to the large eccentric forces applied during rapid braking, which is further accentuated when higher numbers of repetitions are performed. Gradual deceleration zones (> 10 m) are therefore recommended to mitigate undue muscular damage. Performing repeated jumps within the inter-repetition rest period may be an effective strategy to induce a greater physiological stimulus during RST, while exposing athletes to sport-specific actions, without an increase in the volume of high-intensity running [59, 156]. When jumps were prescribed in studies by Buchheit et al. [59] and Padulo et al. [156], very high B[La] (10.2–13.1 m⋅mol−1), HRpeak (96%–97% heart rate max) and sRPE (7.9–8.0 au) were observed. The additional muscular work performed during the recovery period with jumps has previously been shown to increase muscle deoxygenation of the lower limbs, but it should be noted that these sequences are also likely to reduce acute sprint performance [59, 156]. Furthermore, with only two studies investigating the effects of jumps within the inter-repetition rest period, the optimal volume and intensity of these actions are yet to be established. There is potential for other modifications to be implemented during RST, such as sport-specific skills (e.g. passing, shooting), grappling, push-ups and tackling into contact bags. These types of explosive efforts typically precede or follow high-intensity runs/sprints during match play [159,160,161] and may help to better simulate the physiological demands associated with competition. Furthermore, flying sprints that incorporate a submaximal acceleration zone may provide exposure to repeated bouts of maximal velocity sprinting, without the neuromuscular demands of rapid acceleration [162].
4.7 Limitations
There are several important issues to consider when interpreting our findings. Depending on the outcome measure, a proportion of the variation in the meta-analysed acute demands of RST can be explained by factors other than the programming variables investigated (Supplementary Table S4). Factors directly related to individual differences in human physiology have been shown to influence the acute demands to RST, such as age [36, 100, 101, 111, 163,164,165,166], fitness level [167], playing status [46, 168,169,170,171,172,173,174], gender [131, 139, 175, 176] and ethnicity [177]. Furthermore, a proportion of the variation in the acute demands may also be due to the impact of programming variables not investigated (e.g. number of sets), as well varied data collection methods, conditions and reporting. For example, there are inter- and intra-individual differences in B[La] accumulation depending on sampling procedures (time and site), hydration status, previous exercise and ambient temperature [18, 47, 178]. Nevertheless, the influence of the latter factors on the present review are likely to be low considering that item ten in the inclusion–exclusion criteria ensures that RST must have been performed under normal conditions (e.g. hydrated state, ≤ 30 °C) and without fatiguing exercise occurring in the previous 24 h. We also appreciate the concerns of comparing CMJ height between different methods and devices [179], which is why CMJ outcomes were not meta-analysed.
When interpreting acute heart rate and VO2 responses to training, it is important to consider the starting value at the commencement of exercise, which will influence the magnitude of change. However, the majority of studies did not present this information, and thus, we were unable to account for this in our analyses. Additionally, there was an insufficient number of samples to determine the moderating effects of programming variables on average heart rate and VO2. There was also a low number of samples for HRpeak as % HRmax, creatine kinase, spring mass-model parameters and sprint force–velocity–power parameters, which meant we were unable to meta-analyse these outcomes. Therefore, in future, researchers may wish to investigate the effects of RST on these outcomes. Finally, it should be noted that while our elected reference adjustments of 10 m and 10 s allow for comparison between sprint distance and inter-repetition rest time, respectively, this will not always represent the same relative change (i.e. an increased sprint distance from 10 m to 20 m represents a 100% change, while 30 m–40 m represents a 25% change). Therefore, this information should be treated with caution and used within the context of the programmed session.
5 Conclusions
Our systematic review and meta-analysis is the first to summarise the acute physiological, neuromuscular, perceptual and performance demands of RST in team sport athletes, while providing a quantitative synthesis of the effects of programming variables. RST provides a potent physiological stimulus for the physical development of team sport athletes, with the magnitude of the acute demands influenced by several programming variables (Table 4). Longer sprint distances and shorter inter-repetition rest periods are the most efficacious strategies to increase RST demands. When manipulated in combination, these factors are likely to have an even greater effect, from which the magnitude of within-session fatigue and acute training response can be expected to follow. Reducing the number of repetitions per set (e.g. four as opposed to six) can maintain the physiological, perceptual and performance demands of RST while reducing sprint volume. When combined with shorter sprint distances and increased inter-repetition rest periods, this might be a useful strategy during strenuous training and competition periods [26]. Additionally, straight-line, shuttle and multi-directional repeated-sprints can be prescribed to target movement specific outcomes, depending on the aims of the training program. While there is a large quantity of evidence relating to acute performance outcomes of RST, there is a lack of literature on cardiorespiratory (e.g. VO2) and neuromuscular demands. The insights from our review and meta-analysis provide practitioners with the expected demands of RST and can be used to help optimise training prescription through the manipulation of programming variables.
References
Girard O, Mendez-Villanueva A, Bishop D. Repeated-sprint ability—part I. Sports Med. 2011;41(8):673–94.
Taylor JM, Macpherson TW, McLaren SJ, Spears I, Weston M. Two weeks of repeated-sprint training in soccer: to turn or not to turn? Int J Sports Physiol Perform. 2016;11(8):998–1004.
Mendiguchia J, Conceição F, Edouard P, Fonseca M, Pereira R, Lopes H, et al. Sprint versus isolated eccentric training: Comparative effects on hamstring architecture and performance in soccer players. PLoS One. 2020;15(2): e0228283.
Malone S, Roe M, Doran DA, Gabbett TJ, Collins K. High chronic training loads and exposure to bouts of maximal velocity running reduce injury risk in elite Gaelic football. J Sci Med Sport. 2017;20(3):250–4.
Taylor JB, Wright AA, Dischiavi SL, Townsend MA, Marmon AR. Activity demands during multi-directional team sports: a systematic review. Sports Med. 2017;47(12):2533–51.
Bompa TO, Buzzichelli C. Periodization: theory and methodology of training. J Hum Kinet. 2019.
Coffey VG, Hawley JA. The molecular bases of training adaptation. Sports Med. 2007;37(9):737–63.
Taylor J, Macpherson T, Spears I, Weston M. The effects of repeated-sprint training on field-based fitness measures: a meta-analysis of controlled and non-controlled trials. Sports Med. 2015;45(6):881–91.
Manuel Clemente F, Ramirez-Campillo R, Nakamura FY, Sarmento H. Effects of high-intensity interval training in men soccer player’s physical fitness: a systematic review with meta-analysis of randomized-controlled and non-controlled trials. J Sports Sci. 2021;39(11):1202–22.
Boer P, Van Aswegen M. Effect of combined versus repeated sprint training on physical parameters in sub-elite football players in South Africa. J Phys Educ Sport. 2016;16(3):964.
Bravo DF, Impellizzeri FM, Rampinini E, Castagna C, Bishop D, Wisloff U. Sprint vs. interval training in football. Int J Sports Med. 2008;29(08):668–74.
Ross A, Leveritt M. Long-term metabolic and skeletal muscle adaptations to short-sprint training. Sports Med. 2001;31(15):1063–82.
Fernandez-Fernandez J, Zimek R, Wiewelhove T, Ferrauti A. High-intensity interval training vs. repeated-sprint training in tennis. J Strength Cond Res. 2012;26(1):53–62.
Gantois P, Batista GR, Aidar FJ, Nakamura FY, de Lima-Júnior D, Cirilo-Sousa MS, et al. Repeated sprint training improves both anaerobic and aerobic fitness in basketball players. Isokinet Exerc Sci. 2019;27(2):97–105.
Kaynak K, Eryılmaz SK, Aydoğan S, Mihailov D. The effects of 20-m repeated sprint training on aerobic capacity in college volleyball players. Biomed Hum Kinetics. 2017;9(1):43–50.
Maggioni MA, Bonato M, Stahn A, La Torre A, Agnello L, Vernillo G, et al. Effects of ball drills and repeated-sprint-ability training in basketball players. Int J Sports Physiol Perform. 2019;14(6):757–64.
Serpiello FR, McKenna MJ, Bishop DJ, Aughey RJ, Caldow MK, Cameron-Smith D, et al. Repeated sprints alter signaling related to mitochondrial biogenesis in humans. Med Sci Sports Exerc. 2012;44(5):827–34.
Buchheit M, Laursen PB. High-intensity interval training, solutions to the programming puzzle. Part 2: anaerobic energy, neuromuscular load and practical applications. Sports Med. 2013;43:927–54.
Iaia FM, Fiorenza M, Larghi L, Alberti G, Millet GP, Girard O. Short-or long-rest intervals during repeated-sprint training in soccer? PLoS One. 2017;12(2): e0171462.
Beneke R, Leithäuser RM, Ochentel O. Blood lactate diagnostics in exercise testing and training. Int J Sports Physiol Perform. 2011;6(1):8–24.
Krustrup P, Mohr M, Nybo L, Jensen JM, Nielsen JJ, Bangsbo J. The Yo-Yo IR2 test: physiological response, reliability, and application to elite soccer. Med Sci Sports Exerc. 2006;38(9):1666.
Hautier C, Wouassi D, Arsac L, Bitanga E, Thiriet P, Lacour J. Relationships between postcompetition blood lactate concentration and average running velocity over 100-m and 200-m races. Euro J Appl Physiol. 1994;68(6):508–13.
Alemdaroğlu U, Köklü Y, Bektaş F, Çelik G, Ünver F, Duffield R. Comparison of repeated sprint tests in young soccer players: straight versus shuttle. Kinesiol Slov. 2018;24(2):5–16.
Madueno MC, Dalbo VJ, Guy JH, Giamarelos KE, Spiteri T, Scanlan AT. Reduced fatigue in passive versus active recovery: an examination of repeated-change-of-direction sprints in basketball players. Int J Sports Physiol Perform. 2018;13(8):1034–41.
Keir DA, Thériault F, Serresse O. Evaluation of the running-based anaerobic sprint test as a measure of repeated sprint ability in collegiate-level soccer players. J Strength Cond Res. 2013;27(6):1671–8.
Laursen P, Buchheit M. Science and application of high-intensity interval training. J Hum Kinet. 2019.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7): e1000097.
Bishop D, Girard O, Mendez-Villanueva A. Repeated-sprint ability—part II. Sports Med. 2011;41(9):741–56.
Ratel S, Williams C, Oliver J, Armstrong N. Effects of age and recovery duration on performance during multiple treadmill sprints. Int J Sports Med. 2006;27(01):1–8.
Groslambert A, Mahon AD. Perceived exertion. Sports Med. 2006;36(11):911–28.
Girard O, Brocherie F, Bishop D. Sprint performance under heat stress: a review. Scand J Med Sci Sports. 2015;25:79–89.
Doeven SH, Brink MS, Kosse SJ, Lemmink KA. Postmatch recovery of physical performance and biochemical markers in team ball sports: a systematic review. BMJ Open Sport Exerc Med. 2018;4(1): e000264.
Woolley B, Jakeman J, Faulkner J. Multiple sprint exercise with a short deceleration induces muscle damage and performance impairment in young, physically active males. J Athl Enhance. 2014;3:2.
Clifford T, Berntzen B, Davison GW, West DJ, Howatson G, Stevenson EJ. Effects of beetroot juice on recovery of muscle function and performance between bouts of repeated sprint exercise. Nutrients. 2016;8(8):506.
Howatson G, Milak A. Exercise-induced muscle damage following a bout of sport specific repeated sprints. J Strength Cond Res. 2009;23(8):2419–24.
Klatt S, Kossmann M, Hottenrott L, Ferrauti A, Fasold F. Performance changes and recovery time in U20 and older handball players after a high-intensity sprint exercise. Appl Sci. 2021;11(11):5301.
Eryılmaz SK, Aslankeser Z, Özdemir Ç, Özgünen K, Kurdak S. Effects of training load changes on physical performance and exercise-induced muscle damage. Rev Bras Med Esporte. 2019;25:509–14.
López-Segovia M, Pareja-Blanco F, Jiménez-Reyes P, González-Badillo JJ. Determinant factors of repeat sprint sequences in young soccer players. Int J Sports Med. 2015;36(02):130–6.
Lemmink K, Elferink-Gemser M, Visscher C. Evaluation of the reliability of two field hockey specific sprint and dribble tests in young field hockey players. Br J Sports Med. 2004;38(2):138–42.
Johnston RD, Gabbett TJ. Repeated-sprint and effort ability in rugby league players. J Strength Cond Res. 2011;25(10):2789–95.
Austin DJ, Gabbett TJ, Jenkins DG. Reliability and sensitivity of a repeated high-intensity exercise performance test for rugby league and rugby union. J Strength Cond Res. 2013;27(4):1128–35.
Iacono AD, Ardigò LP, Meckel Y, Padulo J. Effect of small-sided games and repeated shuffle sprint training on physical performance in elite handball players. J Strength Cond Res. 2016;30(3):830–40.
Di Mascio M, Ade J, Bradley PS. The reliability, validity and sensitivity of a novel soccer-specific reactive repeated-sprint test (RRST). Eur J Appl Physiol. 2015;115(12):2531–42.
Wragg C, Maxwell N, Doust J. Evaluation of the reliability and validity of a soccer-specific field test of repeated sprint ability. Eur J Appl Physiol. 2000;83(1):77–83.
Di Mascio M, Ade J, Musham C, Girard O, Bradley PS. Soccer-specific reactive repeated-sprint ability in elite youth soccer players: maturation trends and association with various physical performance tests. J Strength Cond Res. 2020;34(12):3538–45.
Brini S, Boullosa D, Calleja-González J, Delextrat A. Construct validity and reliability of a new basketball multidirectional reactive repeated sprint test. Int J Environ Res. 2021;18(20):10695.
Halson SL. Monitoring training load to understand fatigue in athletes. Sports Med. 2014;44(2):139–47.
Morcillo JA, Jiménez-Reyes P, Cuadrado-Peñafiel V, Lozano E, Ortega-Becerra M, Párraga J. Relationships between repeated sprint ability, mechanical parameters, and blood metabolites in professional soccer players. J Strength Cond Res. 2015;29(6):1673–82.
Fitzsimons M, Dawson B, Ward D, Wilkinson A. Cycling and running tests of repeated sprint ability. Aust J Sci Med Sport. 1993;25:82.
Glaister M, Howatson G, Pattison JR, McInnes G. The reliability and validity of fatigue measures during multiple-sprint work: an issue revisited. J Strength Cond Res. 2008;22(5):1597–601.
Lopes-Silva JP, da Silva Santos JF, Abbiss CR, Franchini E. Measurement properties and feasibility of repeated sprint ability test: a systematic review. Strength Cond J. 2019;41(6):41–61.
Samozino P, Rabita G, Dorel S, Slawinski J, Peyrot N, Saez de Villarreal E, et al. A simple method for measuring power, force, velocity properties, and mechanical effectiveness in sprint running. Scand J Med Sci Sports. 2016;26(6):648–58.
Morin J-B, Dalleau G, Kyröläinen H, Jeannin T, Belli A. A simple method for measuring stiffness during running. J Appl Biomech. 2005;21(2):167–80.
Brocherie F, Millet GP, Girard O. Neuro-mechanical and metabolic adjustments to the repeated anaerobic sprint test in professional football players. Eur J Appl Physiol. 2015;115(5):891–903.
McKay AK, Stellingwerff T, Smith ES, Martin DT, Mujika I, Goosey-Tolfrey VL, et al. Defining training and performance caliber: a participant classification framework. Int J Sports Physiol Perform. 2022;1(aop):1–15.
Borg G. The Borg CR Scales Folder. Methods for measuring intensity of experience. Hasselby: Stockholm University; 2010.
Akenhead R, Marques JB, Paul DJ. Accelerometer load: a new way to measure fatigue during repeated sprint training? Sci Med Footb. 2017;1(2):151–6.
Selmi MA, Haj Sassi R, Haj Yahmed M, Moalla W, Elloumi M. Effect of between-set recovery durations on repeated sprint ability in young soccer players. Biol Sport. 2016;33(2):165–72.
Buchheit M. Performance and physiological responses to repeated-sprint and jump sequences. Eur J Appl Physiol. 2010;110(5):1007–18.
Buchheit M, Bishop D, Haydar B, Nakamura FY, Ahmaidi S. Physiological responses to shuttle repeated-sprint running. Int J Sports Med. 2010;31(06):402–9.
Dellal A, Casamichana D, Castellano J, Haddad M, Moalla W, Chamari K. Cardiac parasympathetic reactivation in elite soccer players during different types of traditional high-intensity training exercise modes and specific tests: interests and limits. Asian J Sports Med. 2015;6(4).
Haugen T, Tonnessen E, Leirstein S, Hem E, Seiler S. Not quite so fast: effect of training at 90% sprint speed on maximal and repeated-sprint ability in soccer players. J Sports Sci. 2014;32(20):1979–86.
Till K, Scantlebury S, Jones B. Anthropometric and physical qualities of elite male youth rugby league players. Sports Med. 2017;47(11):2171–86.
Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–84.
Cheung MW-L. A guide to conducting a meta-analysis with non-independent effect sizes. Neuropsychol Rev. 2019;29(4):387–96.
Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth. 2010;1(2):97–111.
Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36(3):1–48.
Pustejovsky J. clubSandwich: Cluster-Robust (Sandwich) Variance Estimators with Small-Sample Corrections. R package version 0.5.3 2021. https://CRAN.R-project.org/package=clubSandwich.
Riley RD. Multivariate meta-analysis: the effect of ignoring within-study correlation. J R Stat Soc A Stat Soc. 2009;172(4):789–811.
IntHout J, Ioannidis JP, Rovers MM, Goeman JJ. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open. 2016;6(7): e010247.
Higgins JP. Commentary: Heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol. 2008;37(5):1158–60.
Viechtbauer W. Confidence intervals for the amount of heterogeneity in meta-analysis. Stat Med. 2007;26(1):37–52.
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. New York: Wiley; 2019.
Greenland S. Valid p-values behave exactly as they should: some misleading criticisms of p-values and their resolution with s-values. Am Stat. 2019;73(sup1):106–14.
Buchheit M. Monitoring training status with HR measures: do all roads lead to Rome? Front Physiol. 2014;5:73.
McLaren SJ. The application of differential ratings of perceived exertion to training monitoring in team sports [Doctoral Thesis]. Middlesbrough: Teesside University; 2018.
Haugen T, Buchheit M. Sprint running performance monitoring: methodological and practical considerations. Sports Med. 2016;46(5):641–56.
Lakomy J, Haydon DT. The effects of enforced, rapid deceleration on performance in a multiple sprint test. J Strength Cond Res. 2004;18(3):579–83.
Buchheit M, Laursen PB. High-intensity interval training, solutions to the programming puzzle. Sports Med. 2013;43(10):927–54.
Harrison PW, Johnston RD. Relationship between training load, fitness, and injury over an Australian rules football preseason. J Strength Cond Res. 2017;31(10):2686–93.
Malone JJ, Di Michele R, Morgans R, Burgess D, Morton JP, Drust B. Seasonal training-load quantification in elite English premier league soccer players. Int J Sports Physiol Perform. 2015;10:489–97.
Dalton-Barron NE, McLaren SJ, Black CJ, Gray M, Jones B, Roe G. Identifying contextual influences on training load: an example in professional Rugby Union. J Strength Cond Res. 2021;35(2):503–11.
Gharbi Z, Dardouri W, Haj-Sassi R, Castagna C, Chamari K, Souissi N. Effect of the number of sprint repetitions on the variation of blood lactate concentration in repeated sprint sessions. Biol Sport. 2014;31(2):151.
Medbø J, Burgers S. Effect of training on the anaerobic capacity. Med Sci Sports Exerc. 1990;22(4):501–7.
Chiu LZ, Barnes JL. The fitness-fatigue model revisited: implications for planning short-and long-term training. J Strength Cond Res. 2003;25(6):42–51.
Dupont G, Millet GP, Guinhouya C, Berthoin S. Relationship between oxygen uptake kinetics and performance in repeated running sprints. Eur J Appl Physiol. 2005;95(1):27–34.
Tønnessen E, Hem E, Leirstein S, Haugen T, Seiler S. Maximal aerobic power characteristics of male professional soccer players, 1989–2012. Int J Sports Physiol Perform. 2013;8(3):323–9.
Haugen TA, Tønnessen E, Hem E, Leirstein S, Seiler S. VO2max characteristics of elite female soccer players, 1989–2007. Int J Sports Physiol Perform. 2014;9(3):515–21.
Gabbett TJ, Jenkins DG, Abernethy B. Relationships between physiological, anthropometric, and skill qualities and playing performance in professional rugby league players. J Sports Sci. 2011;29(15):1655–64.
Higham DG, Pyne DB, Anson JM, Eddy A. Physiological, anthropometric, and performance characteristics of rugby sevens players. Int J Sports Physiol Perform. 2013;8(1):19–27.
Midgley AW, McNaughton LR, Wilkinson M. Is there an optimal training intensity for enhancing the maximal oxygen uptake of distance runners? Sports Med. 2006;36(2):117–32.
Laursen PB, Jenkins DG. The scientific basis for high-intensity interval training. Sports Med. 2002;32(1):53–73.
Midgley A, Mc NL. Time at or near VO2max during continuous and intermittent running: a review with special reference to considerations for the optimisation of training protocols to elicit the longest time at or near VO^ sub 2max. J Sports Med Phys Fit. 2006;46(1):1.
Swain DP, Abernathy KS, Smith CS, Lee SJ, Bunn SA. Target heart rates for the development of cardiorespiratory fitness. Med Sci Sports Exerc. 1994;26(1):112–6.
Aguiar M, Abrantes C, Maçãs V, Leite N, Sampaio J, Ibáñez S. Effects of intermittent or continuous training on speed, jump and repeated-sprint ability in semi-professional soccer players. Open Sports Sci J. 2008;1(1).
Almansba R, Boucher VG, Parent A-A, Comtois AS. Repeated linear and quadrangular sprint as a function of anaerobic power. J Strength Cond Res. 2019;33(8):2177–84.
Brahim MB, Mohamed A, Shalfawi SA. The evaluation of soccer players performance on different repeated sprints tests: training and testing implications. Kinesiol Slov. 2016;22(2).
Brini S, Ben Abderrahman A, Boullosa D, Hackney AC, Zagatto AM, Castagna C, et al. Effects of a 12-week change-of-direction sprints training program on selected physical and physiological parameters in professional basketball male players. Int J Environ Res Public Health. 2020;17(21):8214.
Buchheit M, Haydar B, Ahmaidi S. Repeated sprints with directional changes: do angles matter? J Sports Sci. 2012;30(6):555–62.
Dellal A, Wong DP. Repeated sprint and change-of-direction abilities in soccer players: effects of age group. J Strength Cond Res. 2013;27(9):2504–8.
Gibson N, Currie J, Johnston R, Hill J. Relationship between measures of aerobic fitness, speed and repeated sprint ability in full and part time youth soccer players. J Sports Med Phys Fit. 2013;53(1):9–16.
Gonzalo-Skok O, Tous-Fajardo J, Arjol-Serrano JL, Suarez-Arrones L, Casajús JA, Mendez-Villanueva A. Improvement of repeated-sprint ability and horizontal-jumping performance in elite young basketball players with low-volume repeated-maximal-power training. Int J Sports Physiol Perform. 2016;11(4):464–73.
Perroni F, Corvino M, Cignitti L, Minganti C. RSA response to preseason training in semiprofessional soccer players. Sport Sci Health. 2013;9(2):59–64.
Ruscello B, Tozzo N, Briotti G, Padua E, Ponzetti F, D’Ottavio S. Influence of the number of trials and the exercise to rest ratio in repeated sprint ability, with changes of direction and orientation. J Strength Cond Res. 2013;27(7):1904–19.
Suarez-Arrones L, Tous-Fajardo J, Núñez J, Gonzalo-Skok O, Gálvez J, Mendez-Villanueva A. Concurrent repeated-sprint and resistance training with superimposed vibrations in rugby players. Int J Sports Physiol Perform. 2014;9(4):667–73.
Zagatto AM, Ardigò LP, Barbieri FA, Milioni F, Iacono AD, Camargo BH, et al. Performance and metabolic demand of a new repeated-sprint ability test in basketball players: does the number of changes of direction matter? J Strength Cond Res. 2017;31(9):2438–46.
Zagatto AM, Claus GM, Dutra YM, de Poli RA, Lopes VH, Goodall S, et al. Drop jumps versus sled towing and their effects on repeated sprint ability in young basketball players. BMC Sports Sci Med Rehabil. 2022;14(1):1–11.
Blasco-Lafarga C, Donfrancesco G, Montoya-Vieco A, Cordellat A, Monteagudo P, Roldán A, et al. Quantifying performance impairment, specificity and fatigue in young soccer professionals: UirFide Soccer test vs. Bangsbo test. Gazz Med Ital Arch Sci Med. 2020;179(7–8):437–47.
Kaplan T. Examination of repeated sprinting ability and fatigue index of soccer players according to their positions. J Strength Cond Res. 2010;24(6):1495–501.
Joo CH. The effects of short-term detraining on exercise performance in soccer players. J Exerc Rehabil. 2016;12(1):54–9.
Turki O, Dhahbi W, Gueid S, Hmaied S, Souaifi M, Khalifa R. Dynamic warm-up with a weighted vest: improvement of repeated change-of-direction performance in young male soccer players. Int J Sport Physiol Perform. 2020;15(2):196–203.
Brughelli M, Cronin J, Levin G, Chaouachi A. Understanding change of direction ability in sport. Sports Med. 2008;38(12):1045–63.
Sheppard JM, Young WB. Agility literature review: classifications, training and testing. J Sports Sci. 2006;24(9):919–32.
Padulo J, Laffaye G, Haddad M, Chaouachi A, Attene G, Migliaccio GM, et al. Repeated sprint ability in young basketball players: one vs. two changes of direction (Part 1). J Sports Sci. 2015;33(14):1480–92.
Attene G, Nikolaidis PT, Bragazzi NL, Dello Iacono A, Pizzolato F, Zagatto AM, et al. Repeated sprint ability in young basketball players (Part 2): the chronic effects of multidirection and of one change of direction are comparable in terms of physiological and performance responses. Front Physiol. 2016;7:262.
Dal Pupo J, Detanico D, Carminatti LJ, Santos SG. Physiological and neuromuscular responses in the shuttle and straight line-repeated sprint running. Apunts Med Esport. 2013;48(178):43–8.
Sánchez-Sánchez J, García-Unanue J, Jiménez-Reyes P, Gallardo A, Burillo P, Felipe JL, et al. Influence of the mechanical properties of third-generation artificial turf systems on soccer players’ physiological and physical performance and their perceptions. PLoS One. 2014;9(10): e111368.
Abt G, Siegler JC, Akubat I, Castagna C. The effects of a constant sprint-to-rest ratio and recovery mode on repeated sprint performance. J Strength Cond Res. 2011;25(6):1695–702.
Figueira B, Gonçalves B, Abade E, Paulauskas R, Masiulis N, Kamarauskas P, et al. Repeated sprint ability in elite basketball players: the effects of 10× 30 m vs. 20× 15 m exercise protocols on physiological variables and sprint performance. J Hum Kinet. 2021;77(1):181–9.
Iaia FM, Fiorenza M, Perri E, Alberti G, Millet GP, Bangsbo J. The effect of two speed endurance training regimes on performance of soccer players. PLoS One. 2015;10(9): e0138096.
Little T, Williams AG. Effects of sprint duration and exercise: rest ratio on repeated sprint performance and physiological responses in professional soccer players. J Strength Cond Res. 2007;21(2):646–8.
Paulauskas R, Kamarauskas P, Nekriošius R, Bigwood NM. Physical and physiological response to different modes of repeated sprint exercises in basketball players. J Hum Kinet. 2020;72(1):91–9.
Russell M, Birch J, Love T, Cook CJ, Bracken RM, Taylor T, et al. The effects of a single whole-body cryotherapy exposure on physiological, performance, and perceptual responses of professional academy soccer players after repeated sprint exercise. J Strength Cond Res. 2017;31(2):415–21.
Eliakim M, Meckel Y, Gotlieb R, Nemet D, Eliakim A. Motivational music and repeated sprint ability in junior basketball players. Acta Kinesiologiae Universitatis Tartuensis. 2012;18:29–38.
Ulupınar S, Hazır T, Kinİşler A. The contribution of energy systems in repeated-sprint protocols: The effect of distance, rest, and repetition. Res Q Exerc Sport. 2023;94:173–9.
Ulupınar S, Özbay S, Gençoğlu C, Franchini E, Kishalı NF, İnce İ. Effects of sprint distance and repetition number on energy system contributions in soccer players. J Exerc Sci Fit. 2021;19(3):182–8.
Costello SE, O’Neill BV, Howatson G, van Someren K, Haskell-Ramsay CF. Detrimental effects on executive function and mood following consecutive days of repeated high-intensity sprint interval exercise in trained male sports players. J Sports Sci. 2022;40:783–96.
Haugen T, Tønnessen E, Øksenholt Ø, Haugen FL, Paulsen G, Enoksen E, et al. Sprint conditioning of junior soccer players: effects of training intensity and technique supervision. PLoS One. 2015;10(3): e0121827.
Spencer M, Lawrence S, Rechichi C, Bishop D, Dawson B, Goodman C. Time–motion analysis of elite field hockey, with special reference to repeated-sprint activity. J Sports Sci. 2004;22(9):843–50.
Dawson B. Repeated-sprint ability: where are we? Int J Sports Physiol Perform. 2012;7(3):285–9.
Dent JR, Edge JA, Hawke E, McMahon C, Mündel T. Sex differences in acute translational repressor 4E-BP1 activity and sprint performance in response to repeated-sprint exercise in team sport athletes. J Sci Med Sport. 2015;18(6):730–6.
Vollaard N, Metcalfe R, Williams S. Effect of number of sprints in a SIT session on change in VO2max: a meta-analysis. Med Sci Sports Exerc. 2017;49(6):1147–56.
Mendez-Villanueva A, Hamer P, Bishop D. Fatigue in repeated-sprint exercise is related to muscle power factors and reduced neuromuscular activity. Eur J Appl Physiol. 2008;103(4):411–9.
Sandford GN, Laursen PB, Buchheit M. Anaerobic speed/power reserve and sport performance: scientific basis, current applications and future directions. Sports Med. 2021;51(10):2017–28.
Julio UF, Panissa VL, Paludo AC, Alves ED, Campos FA, Franchini E. Use of the anaerobic speed reserve to normalize the prescription of high-intensity interval exercise intensity. Eur J Sport Sci. 2020;20(2):166–73.
Spencer M, Bishop D, Dawson B, Goodman C. Physiological and metabolic responses of repeated-sprint activities. Sports Med. 2005;35(12):1025–44.
Jiménez-Reyes P, Garcia-Ramos A, Párraga-Montilla JA, Morcillo-Losa JA, Cuadrado-Peñafiel V, Castaño-Zambudio A, et al. Seasonal changes in the sprint acceleration force-velocity profile of elite male soccer players. J Strength Cond Res. 2022;36(1):70–4.
Jiménez-Reyes P, García-Ramos A, Cuadrado-Peñafiel V, Párraga-Montilla JA, Morcillo-Losa JA, Samozino P, et al. Differences in sprint mechanical force–velocity profile between trained soccer and futsal players. Int J Sports Physiol Perform. 2019;14(4):478–85.
Mancha-Triguero D, García-Rubio J, Gamonales JM, Ibáñez SJ. Strength and speed profiles based on age and sex differences in young basketball players. Int J Environ Res Public Health. 2021;18(2):643.
Izquierdo M, Ibañez J, González-Badillo JJ, Gorostiaga EM. Effects of creatine supplementation on muscle power, endurance, and sprint performance. Med Sci Sports Exerc. 2002;34(2):332–43.
Broderick V, Uiga L, Driller M. Flotation-restricted environmental stimulation therapy improves sleep and performance recovery in athletes. Perform Enhancement Health. 2019;7(1–2).
Conte D, Favero TG, Lupo C, Francioni FM, Capranica L, Tessitore A. Time-motion analysis of Italian elite women’s basketball games: individual and team analyses. J Strength Cond Res. 2015;29(1):144–50.
Manchado C, Pers J, Navarro F, Han A, Sung E, Platen P. Time-motion analysis in women’s team handball: importance of aerobic performance. J Hum Sport Exerc. 2013.
Mero A, Komi P, Gregor R. Biomechanics of sprint running. Sports Med. 1992;13(6):376–92.
Higashihara A, Nagano Y, Ono T, Fukubayashi T. Differences in hamstring activation characteristics between the acceleration and maximum-speed phases of sprinting. J Sports Sci. 2018;36(12):1313–8.
Timmins RG, Opar DA, Williams MD, Schache AG, Dear NM, Shield AJ. Reduced biceps femoris myoelectrical activity influences eccentric knee flexor weakness after repeat sprint running. Scand J Med Sci Sports. 2014;24(4):e299–305.
Thelen DG, Chumanov ES, Hoerth DM, Best TM, Swanson SC, Li L, et al. Hamstring muscle kinematics during treadmill sprinting. Med Sci Sports Exerc. 2005;37(1):108–14.
Schache AG, Dorn TW, Blanch PD, Brown NA, Pandy MG. Mechanics of the human hamstring muscles during sprinting. Med Sci Sports Exerc. 2012;44(4):647–58.
Girard O, Racinais S, Kelly L, Millet GP, Brocherie F. Repeated sprinting on natural grass impairs vertical stiffness but does not alter plantar loading in soccer players. Eur J Appl Physiol. 2011;111(10):2547–55.
Padulo J, Tabben M, Ardigò L, Ionel M, Popa C, Gevat C, et al. Repeated sprint ability related to recovery time in young soccer players. Res Sports Med. 2015;23(4):412–23.
Balsom P, Seger J, Sjödin B, Ekblom B. Maximal-intensity intermittent exercise: effect of recovery duration. Int J Sports Med. 1992;13(07):528–33.
Tabata I, Nishimura K, Kouzaki M, Hirai Y, Ogita F, Miyachi M, et al. Effects of moderate-intensity endurance and high-intensity intermittent training on anaerobic capacity and VO2max. Med Sci Sports Exerc. 1996;28:1327–30.
Castagna C, Abt G, Manzi V, Annino G, Padua E, D’Ottavio S. Effect of recovery mode on repeated sprint ability in young basketball players. J Strength Cond Res. 2008;22(3):923–9.
Brini S, Ahmaidi S, Bouassida A. Effects of passive versus active recovery at different intensities on repeated sprint performance and testosterone/cortisol ratio in male senior basketball players. Sci Sports. 2020;35(5):e142–7.
Dupont G, Berthoin S. Time spent at a high percentage of max for short intermittent runs: active versus passive recovery. Can J Appl Physiol. 2004;29(S1):S3–16.
Padulo J, Tabben M, Attene G, Ardigò L, Dhahbi W, Chamari K. The impact of jumping during recovery on repeated sprint ability in young soccer players. Res Sports Med. 2015;23(3):240–52.
Buchheit M, Cormie P, Abbiss C, Ahmaidi S, Nosaka KK, Laursen P. Muscle deoxygenation during repeated sprint running: effect of active vs. passive recovery. Int J Sports Med. 2009;30(06):418–25.
Dupont G, Moalla W, Guinhouya C, Ahmaidi S, Berthoin S. Passive versus active recovery during high-intensity intermittent exercises. Med Sci Sports Exerc. 2004;36(2):302–8.
Austin DJ, Gabbett TJ, Jenkins DJ. Repeated high-intensity exercise in a professional rugby league. J Strength Cond Res. 2011;25(7):1898–904.
Carling C, Le Gall F, Dupont G. Analysis of repeated high-intensity running performance in professional soccer. J Sports Sci. 2012;30(4):325–36.
Sirotic AC, Coutts AJ, Knowles H, Catterick C. A comparison of match demands between elite and semi-elite rugby league competition. J Sports Sci. 2009;27(3):203–11.
Beato M, Drust B. Acceleration intensity is an important contributor to the external and internal training load demands of repeated sprint exercises in soccer players. Res Sports Med. 2021;29(1):67–76.
Lockie RG, Davis DL, Birmingham-Babauta SA, Beiley MD, Hurley JM, Stage AA, et al. Physiological characteristics of incoming freshmen field players in a men’s Division I collegiate soccer team. Sports. 2016;4(2):34.
Mujika I, Spencer M, Santisteban J, Goiriena JJ, Bishop D. Age-related differences in repeated-sprint ability in highly trained youth football players. J Sports Sci. 2009;27(14):1581–90.
Rodríguez-Fernández A, Sánchez-Sánchez J, Ramirez-Campillo R, Rodríguez-Marroyo JA, Villa Vicente JG, Nakamura FY. Effects of short-term in-season break detraining on repeated-sprint ability and intermittent endurance according to initial performance of soccer player. PLoS One. 2018;13(8): e0201111.
Jorge G, Garrafoli MT, Abad CCC. Seasonal repeated sprint ability with change of direction variations in U17 and U20 elite Brazilian soccer players: a comparative study. J Strength Cond Res. 2020;34(5):1431–9.
Alizadeh R, Hovanloo F, Safania AM. The relationship between aerobic power and repeated sprint ability in young soccer players with different levels of VO2 max. J Phys Educ Sport. 2010;27(2).
Campa F, Semprini G, Júdice PB, Messina G, Toselli S. Anthropometry, physical and movement features, and repeated-sprint ability in soccer players. Int J Sports Med. 2019;40(02):100–9.
García-Unanue J, Felipe JL, Bishop D, Colino E, Ubago-Guisado E, López-Fernández J, et al. Muscular and physical response to an agility and repeated sprint tests according to the level of competition in futsal players. Front Psychol. 2020;11:3671.
Impellizzeri F, Rampinini E, Castagna C, Bishop D, Bravo DF, Tibaudi A, et al. Validity of a repeated-sprint test for football. Int J Sports Med. 2008;29(11):899–905.
Ingebrigtsen J, Bendiksen M, Randers MB, Castagna C, Krustrup P, Holtermann A. Yo-Yo IR2 testing of elite and sub-elite soccer players: performance, heart rate response and correlations to other interval tests. J Sports Sci. 2012;30(13):1337–45.
Keogh JW, Weber CL, Dalton CT. Evaluation of anthropometric, physiological, and skill-related tests for talent identification in female field hockey. Can J Appl Physiol. 2003;28(3):397–409.
Le Rossignol P, Gabbett TJ, Comerford D, Stanton WR. Repeated-sprint ability and team selection in Australian football league players. Int J Sports Physiol Perform. 2014;9(1):161–5.
Rampinini E, Sassi A, Morelli A, Mazzoni S, Fanchini M, Coutts AJ. Repeated-sprint ability in professional and amateur soccer players. Appl Physiol Nutr Metab. 2009;34(6):1048–54.
Delextrat A, Calleja-González J, Hippocrate A, Clarke ND. Effects of sports massage and intermittent cold-water immersion on recovery from matches by basketball players. J Sports Sci. 2013;31(1):11–9.
Tounsi M, Jaafar H, Aloui A, Tabka Z, Trabelsi Y. Effect of listening to music on repeated-sprint performance and affective load in young male and female soccer players. Sport Sci Health. 2019;15(2):337–42.
Galy O, Zongo P, Chamari K, Chaouachi A, Michalak E, Dellal A, et al. Anthropometric and physiological characteristics of Melanesian futsal players: a first approach to talent identification in Oceania. Biol Sport. 2015;32(2):135.
Krustrup P, Mohr M, Steensberg A, Bencke J, Kjær M, Bangsbo J. Muscle and blood metabolites during a soccer game: implications for sprint performance. Med Sci Sports Exerc. 2006;38(6):1165–74.
McMahon JJ, Jones PA, Comfort P. Comment on: “Anthropometric and physical qualities of elite male youth rugby league players.” Sports Med. 2017;47(12):2667–8.
AbuMoh’d MF, Abubaker M. Effect of β-alanine supplementation on repeated sprint ability and responses of blood lactate and bicarbonate in male soccer players. Sport Mont. 2020;18(2):83–8.
Altimari JM, Altimari LR, Bortolotti H, Junior AF, Gabardo JM, Buzzachera CF, et al. The relative age effect on anthropometry, body composition, biological maturation and motor performance in young Brazilian soccer players. J Hum Kinet. 2021;77(1):147–57.
Archiza B, Andaku DK, Caruso FCR, Bonjorno JC Jr, Oliveira CR, Ricci PA, et al. Effects of inspiratory muscle training in professional women football players: a randomized sham-controlled trial. J Sports Sci. 2018;36(7):771–80.
Ayarra R, Nakamura FY, Iturricastillo A, Castillo D, Yanci J. Differences in physical performance according to the competitive level in futsal players. J Hum Kinet. 2018;64:275.
Aziz A, Chia M, Teh K. The relationship between maximal oxygen uptake and repeated sprint performance indices in field hockey and soccer players. J Sports Med Phys Fit. 2000;40(3):195.
Baldi M, Da Silva JF, Buzachera C, Castagna C, Guglielmo LG. Repeated sprint ability in soccer players: associations with physiological and neuromuscular factors. J Sports Med Phys Fit. 2017;57:26–32.
Balsalobre-Fernández C, Tejero-González CM, del Campo-Vecino J, Bachero-Mena B, Sánchez-Martínez J. Relationships among repeated sprint ability, vertical jump performance and upper-body strength in professional basketball players. Arch Med Deporte. 2014;31(161):148–53.
Beato M, Coratella G, Bianchi M, Costa E, Merlini M. Short-term repeated-sprint training (straight sprint vs. changes of direction) in soccer players. J Hum Kinet. 2019;70:183.
Beato M, Bianchi M, Coratella G, Merlini M, Drust B. A single session of straight line and change-of-direction sprinting per week does not lead to different fitness improvements in elite young soccer players. J Strength Cond Res. 2022;36(2):518–24.
Beaven CM, Kilduff LP, Cook CJ. Lower-limb passive heat maintenance combined with pre-cooling improves repeated sprint ability. Front Physiol. 2018;9:1064.
Binnie MJ, Dawson B, Arnot MA, Pinnington H, Landers G, Peeling P. Effect of sand versus grass training surfaces during an 8-week pre-season conditioning programme in team sport athletes. J Sports Sci. 2014;32(11):1001–12.
Binnie MJ, Dawson B, Pinnington H, Landers G, Peeling P. Effect of training surface on acute physiological responses after interval training. J Strength Cond Res. 2013;27(4):1047–56.
Binnie MJ, Dawson B, Pinnington H, Landers G, Peeling P. Part 2: Effect of training surface on acute physiological responses after sport-specific training. J Strength Cond Res. 2013;27(4):1057–66.
Borges JH, Conceição MS, Vechin FC, Pascoal EHF, Silva RP, Borin JP. The effects of resisted sprint vs. plyometric training on sprint performance and repeated sprint ability during the final weeks of the youth soccer season. Sci Sports. 2016;31(4): e101-e5.
Brini S, Marzouki H, Castagna C, Bouassida A. Effects of a four-week small-sided game and repeated sprint ability training during and after Ramadan on aerobic and anaerobic capacities in senior basketball players. Ann Appl Sport Sci. 2018;6(3):7–13.
Brini S, Delextrat A, Bouassida A. Variation in lower limb power and three point shot performance following repeated sprints: one vs. five changes of direction in male basketball players. J Hum Kinet. 2021;77(1):169–79.
Brocherie F, Girard O, Forchino F, Al Haddad H, Dos Santos GA, Millet GP. Relationships between anthropometric measures and athletic performance, with special reference to repeated-sprint ability, in the Qatar national soccer team. J Sports Sci. 2014;32(13):1243–54.
Brocherie F, Millet GP, Hauser A, Steiner T, Rysman J, Wehrlin JP, et al. “Live high-train low and high” hypoxic training improves team-sport performance. Med Sci Sports Exerc. 2015;47(10):2140–9.
Buchheit M. Repeated-sprint performance in team sport players: associations with measures of aerobic fitness, metabolic control and locomotor function. Int J Sports Med. 2012;33(03):230–9.
Campos FDS, Borszcz FK, Flores LJF, Barazetti LK, Teixeira AS, Hartmann Nunes RF, et al. HIIT models in addition to training load and heart rate variability are related with physiological and performance adaptations after 10-weeks of training in young futsal players. Front Psychol. 2021;12: 636153.
Campos-Vazquez MA, Romero-Boza S, Toscano-Bendala FJ, Leon-Prados JA, Suarez-Arrones LJ, Gonzalez-Jurado JA. Comparison of the effect of repeated-sprint training combined with two different methods of strength training on young soccer players. J Strength Cond Res. 2015;29(3):744–51.
Caprino D, Clarke ND, Delextrat A. The effect of an official match on repeated sprint ability in junior basketball players. J Sports Sci. 2012;30(11):1165–73.
Castagna C, Manzi V, D’ottavio S, Annino G, Padua E, Bishop D. Relation between maximal aerobic power and the ability to repeat sprints in young basketball players. J Strength Cond Res. 2007;21(4):1172–6.
Chaouachi A, Manzi V, Wong DP, Chaalali A, Laurencelle L, Chamari K, et al. Intermittent endurance and repeated sprint ability in soccer players. J Strength Cond Res. 2010;24(10):2663–9.
Charlot K, Zongo P, Leicht AS, Hue O, Galy O. Intensity, recovery kinetics and well-being indices are not altered during an official FIFA futsal tournament in Oceanian players. J Sports Sci. 2016;34(4):379–88.
Chen Y-S, Lu W-A, Clemente FM, Bezerra JP, Kuo C-D. Increased parasympathetic activity by foot reflexology massage after repeated sprint test in collegiate football players: a randomised controlled trial. Sports. 2019;7(11):228.
Corrêa DA, Soares DS, Gonelli PR, Cesar MC, Germano MD, Sindorf MA, et al. Effect of 29 weeks of periodized soccer training on the neuromuscular performance of soccer players under 20 years of age. J Exerc Physiol Online. 2016;19(4):32–42.
Cuadrado-Peñafiel V, Párraga-Montilla J, Ortega-Becerra MA, Jiménez-Reyes P. Repeated sprint ability in professional soccer vs. professional futsal players. J Sports Sci. 2014;10(2):89–98.
da Silva JF, Guglielmo LG, Bishop D. Relationship between different measures of aerobic fitness and repeated-sprint ability in elite soccer players. J Strength Cond Res. 2010;24(8):2115–21.
Dal Pupo J, Detanico D, Arins FB, Nascimento Salvador PC, Guglielmo LGA, dos Santos SG. Repeated sprint ability and muscle power levels of the futsal players of U15 and U17 categories. Rev Bras Cienc Esporte. 2017;39(1):73–8.
Daneshfar A, Gahreman DE, Koozehchian MS, Amani Shalamzari S, Hassanzadeh Sablouei M, Rosemann T, et al. Multi directional repeated sprint is a valid and reliable test for assessment of junior handball players. Front Physiol. 2018;9:317.
Dardouri W, Selmi MA, Sassi RH, Gharbi Z, Rebhi A, Yahmed MH, et al. Relationship between repeated sprint performance and both aerobic and anaerobic fitness. J Hum Kinet. 2014;40(1):139–48.
de Andrade VL, Palucci Vieira LH, Kalva-Filho CA, Santiago PRP. Critical points of performance in repeated sprint: a kinematic approach. Sci Sports. 2021.
Delextrat A, Hippocrate A, Leddington-Wright S, Clarke ND. Including stretches to a massage routine improves recovery from official matches in basketball players. J Strength Cond Res. 2014;28(3):716–27.
Delextrat A, Kraiem S. Heart-rate responses by playing position during ball drills in basketball. Int J Sports Physiol Perform. 2013;8(4):410–8.
Donghi F, Rampinini E, Bosio A, Fanchini M, Carlomagno D, Maffiuletti NA. Morning priming exercise strategy to enhance afternoon performance in young elite soccer players. Int J Sports Physiol Perform. 2021;16(3):407–14.
Doyle B, Browne D, Horan D. The relationship of aerobic endurance and linear speed on repeat sprint ability performance in female international footballers. Sciences. 2020;8(4):147–53.
Dupont G, McCall A, Prieur F, Millet GP, Berthoin S, Millet GP. Faster oxygen uptake kinetics during recovery is related to better repeated sprinting ability. Eur J Appl Physiol. 2010;110(3):627–34.
Elias GP, Varley MC, Wyckelsma VL, McKenna MJ, Minahan CL, Aughey RJ. Effects of water immersion on posttraining recovery in Australian footballers. Int J Sports Physiol Perform. 2012;7(4):357–66.
Elias GP, Wyckelsma VL, Varley MC, McKenna MJ, Aughey RJ. Effectiveness of water immersion on postmatch recovery in elite professional footballers. Int J Sports Physiol Perform. 2013;8(3):243–53.
Eniseler N, Şahan Ç, Özcan I, Dinler K. High-intensity small-sided games versus repeated sprint training in junior soccer players. J Hum Kinet. 2017;60:101.
Eryılmaz SK, Kaynak K. Relationship between repeated sprint ability and aerobic fitness in college volleyball players. Univers J Educ Res. 2019;7(5):1198–204.
Essid S, Cherif M, Chtourou H, Souissi N. Time-of-day effects in physical performances and psychological responses in young elite male handball players. Biol Rhythm Res. 2021:1–12.
Farjallah MA, Hammouda O, Ben Mahmoud L, Graja A, Ghattassi K, Boudaya M, et al. Melatonin supplementation ameliorates oxidative stress, antioxidant status and physical performances recovery during a soccer training camp. Biol Rhythm Res. 2020;51(3):441–52.
Fornasier-Santos C, Millet GP, Woorons X. Repeated-sprint training in hypoxia induced by voluntary hypoventilation improves running repeated-sprint ability in rugby players. Eur J Sport Sci. 2018;18(4):504–12.
Fort-Vanmeerhaeghe A, Montalvo A, Latinjak A, Unnithan V. Physical characteristics of elite adolescent female basketball players and their relationship to match performance. J Hum Kinet. 2016;53:167.
Fortin J-F, Billaut F. Blood-flow restricted warm-up alters muscle hemodynamics and oxygenation during repeated sprints in American football players. Sports (Basel). 2019;7(5).
Freitas TT, Calleja-González J, Alarcón F, Alcaraz PE. Acute effects of two different resistance circuit training protocols on performance and perceived exertion in semiprofessional basketball players. J Strength Cond Res. 2016;30(2):407–14.
Gabbett TJ. The development of a test of repeated-sprint ability for elite women’s soccer players. J Strength Cond Res. 2010;24(5):1191–4.
Gabbett T, Jenkins D, Abernethy B. Relative importance of physiological, anthropometric, and skill qualities to team selection in professional rugby league. J Sports Sci. 2011;29(13):1453–61.
Gabbett TJ, Carius J, Mulvey M. Does improved decision-making ability reduce the physiological demands of game-based activities in field sport athletes? J Strength Cond Res. 2008;22(6):2027–35.
Galvin HM, Cooke K, Sumners DP, Mileva KN, Bowtell JL. Repeated sprint training in normobaric hypoxia. Br J Sports Med. 2013;47(Suppl 1):i74–9.
Gantois P, Aidar FJ, De Matos DG, De Souza RF, Da Silva LM, De Castro KR, et al. Repeated sprints and the relationship with anaerobic and aerobic fitness of basketball athletes. J Phys Educ Sport. 2017;17(2):910.
Gantois P, Aidar FJ, Dantas MP, Silva LM, Paes PP, Santana EE, et al. Aerobic fitness is associated with improved repeated sprints ability of basketball players after six weeks of training during preseason. Rev Bras Cineantropometria Desempenho Humano. 2018;20:114–24.
Gatterer H, Klarod K, Heinrich D, Schlemmer P, Dilitz S, Burtscher M. Effects of a 12-day maximal shuttle-run shock microcycle in hypoxia on soccer specific performance and oxidative stress. Appl Physiol. 2015;40(8):842–5.
Gharbi Z, Dardouri W, Haj-Sassi R, Chamari K, Souissi N. Aerobic and anaerobic determinants of repeated sprint ability in team sports athletes. Biol Sport. 2015;32(3):207.
Girard O, Millet GP, Thomson A, Brocherie F. Is plantar loading altered during repeated sprints on artificial turf in international football players? J Sports Sci Med. 2018;17(3):359.
González-Frutos P, Aguilar-Navarro M, Morencos E, Mallo J, Veiga S. Relationships between strength and step frequency with fatigue index in repeated sprint ability. Int J Environ Res Public Health. 2022;19(1):196.
Goodall S, Charlton K, Howatson G, Thomas K. Neuromuscular fatigability during repeated-sprint exercise in male athletes. Med Sci Sports Exerc. 2015;47(3):528–36.
Hamlin MJ. The effect of contrast temperature water therapy on repeated sprint performance. J Sci Med Sport. 2007;10(6):398–402.
Hamlin MJ, Olsen PD, Marshall HC, Lizamore CA, Elliot CA. Hypoxic repeat sprint training improves rugby player’s repeated sprint but not endurance performance. Front Physiol. 2017;8:24.
Hammami M, Gaamouri N, Aloui G, Shephard RJ, Chelly MS. Effects of a complex strength-training program on athletic performance of junior female handball players. Int J Sports Physiol Perform. 2019;14(2):163–9.
Hermassi S, Schwesig R, Wollny R, Fieseler G, Fernandez-Fernandez J, Shephard R, et al. Shuttle versus straight repeated-sprint ability tests and their relationship to anthropometrics and explosive muscular performance in elite handball players. J Sports Med Phys Fit. 2018;58(11):1625–34.
Hollville E, Le Croller V, Hirasawa Y, Husson R, Rabita G, Brocherie F. Effect of prior fatiguing sport-specific exercise on field Hockey passing ability. Int J Sports Physiol Perform. 2018:1–7.
Ingebrigtsen J, Brochmann M, Castagna C, Bradley PS, Ade J, Krustrup P, et al. Relationships between field performance tests in high-level soccer players. J Strength Cond Res. 2014;28(4):942–9.
Jang JH, Joo CH. The effects of residential environment on the condition and fitness of soccer players in the summer. J Exerc Rehabil. 2020;16(6):522–8.
Jiménez-Reyes P, Cross M, Ross A, Samozino P, Brughelli M, Gill N, et al. Changes in mechanical properties of sprinting during repeated sprint in elite rugby sevens athletes. Eur J Sport Sci. 2019;19(5):585–94.
Jorge G, Garrafoli MT, Cal Abad CC. Seasonal repeated sprint ability with change of direction variations in U17 and U20 elite Brazilian soccer players: a comparative study. J Strength Cond Res. 2020;34(5):1431–9.
Kilduff LP, West DJ, Williams N, Cook CJ. The influence of passive heat maintenance on lower body power output and repeated sprint performance in professional rugby league players. J Sci Med Sport. 2013;16(5):482–6.
Krakan I, Milanovic L, Belcic I. Effects of plyometric and repeated sprint training on physical performance. Sports. 2020;8(7):91.
Krueger M, Costello JT, Stenzel M, Mester J, Wahl P. The physiological effects of daily cold-water immersion on 5-day tournament performance in international standard youth field-hockey players. Eur J Appl Physiol. 2020;120(1):295–305.
Lapointe J, Paradis-Deschênes P, Woorons X, Lemaître F, Billaut F. Impact of hypoventilation training on muscle oxygenation, myoelectrical changes, systemic [K+], and repeated-sprint ability in basketball players. Front Sports Act. 2020;2:29.
Lockie RG, Davis DL, Birmingham-Babauta SA, Beiley MD, Hurley JM, Stage AA, et al. Physiological characteristics of incoming freshmen field players in a men's division I collegiate soccer team. Sports (Basel). 2016;4(2).
Lockie RG, Liu TM, Stage AA, Lazar A, Giuliano DV, Hurley JM, et al. Assessing repeated-sprint ability in division I collegiate women soccer players. J Strength Cond Res. 2020;34(7):2015–23.
Lockie RG, Moreno MR, Orjalo AJ, Stage AA, Liu TM, Birmingham-Babauta SA, et al. Repeated-sprint ability in division I collegiate male soccer players: positional differences and relationships with performance tests. J Strength Cond Res. 2019;33(5):1362–70.
Lombard WP, Cai X, Lambert MI, Chen X, Mao L. Relationships between physiological characteristics and match demands in elite-level male field hockey players. Int J Sports Sci Coach. 2021.
Marcelino P, Aoki M, Arruda A, Freitas C, Mendez-Villanueva A, Moreira A. Does small-sided-games’ court area influence metabolic, perceptual, and physical performance parameters of young elite basketball players? Biol Sport. 2016;33(1):37.
Matzenbacher F, Pasquarelli BN, Rabelo FN, Dourado AC, Durigan JZ, Rossi HG, et al. Adaptations in the physical capacities of U-18 futsal athletes during a competitive season. Rev Bras Cineantropometria Desempenho Hum. 2016;18(1):50–61.
McGawley K, Andersson PI. The order of concurrent training does not affect soccer-related performance adaptations. Int J Sports Med. 2013;34(11):983–90.
Meckel Y, Doron O, Eliakim E, Eliakim A. Seasonal variations in physical fitness and performance indices of elite soccer players. Sports. 2018;6(1):14.
Meckel Y, Gottlieb R, Eliakim A. Repeated sprint tests in young basketball players at different game stages. Eur J Appl Physiol. 2009;107(3):273.
Meckel Y, Machnai O, Eliakim A. Relationship among repeated sprint tests, aerobic fitness, and anaerobic fitness in elite adolescent soccer players. J Strength Cond Res. 2009;23(1):163–9.
Meckel Y, May-rom M, Ekshtien A, Eisenstein T, Nemet D, Eliakim A. Relationships among two repeated activity tests and aerobic fitness of volleyball players. J Strength Cond Res. 2015;29(8):2122–7.
Meckel Y, Einy A, Gottlieb R, Eliakim A. Repeated sprint ability in young soccer players at different game stages. J Strength Cond Res. 2014;28(9):2578–84.
Michalsik LB, Madsen K, Aagaard P. Physiological capacity and physical testing in male elite team handball. J Sports Med Phys Fit. 2015;55(5):415–29.
Mohr M, Draganidis D, Chatzinikolaou A, Barbero-Álvarez JC, Castagna C, Douroudos I, et al. Muscle damage, inflammatory, immune and performance responses to three football games in 1 week in competitive male players. Eur J Appl Physiol. 2016;116(1):179–93.
Mohr M, Krustrup P. Comparison between two types of anaerobic speed endurance training in competitive soccer players. J Hum Kinet. 2016;51(1):183–92.
Mohr M, Nybo L, Grantham J, Racinais S. Physiological responses and physical performance during football in the heat. PLoS One. 2012;7(6).
Moncef C, Said M, Olfa N, Dagbaji G. Influence of morphological characteristics on physical and physiological performances of Tunisian elite male handball players. Asian J Sports Med. 2012;3(2):74–80.
Moreira A, Costa EC, Coutts AJ, Nakamura FY, da Silva DA, Aoki MS. Cold water immersion did not accelerate recovery after a futsal match. Rev Bras Med Esporte. 2015.
Müller CB, da Veiga RS, dos Santos PE, Del Vecchio FB. Acute effects of running anaerobic-based sprint test with different loads in amateur rugby union players. Sci Sports. 2021;36(1):85–8.
Okuno NM, Tricoli V, Silva SB, Bertuzzi R, Moreira A, Kiss MA. Postactivation potentiation on repeated-sprint ability in elite handball players. J Strength Cond Res. 2013;27(3):662–8.
Nakamura F, Soares-Caldeira L, Laursen P, Polito M, Leme L, Buchheit M. Cardiac autonomic responses to repeated shuttle sprints. Int J Sports Med. 2009;30(11):808–13.
Nascimento PC, Lucas RDD, Pupo JD, Arins FB, Castagna C, Guglielmo LGA. Effects of four weeks of repeated sprint training on physiological indices in futsal players. Rev Bras Cineantropometria Desempenho Hum. 2015;17(1):91–103.
Nedrehagen ES, Saeterbakken AH. The effects of in-season repeated sprint training compared to regular soccer training. J Hum Kinet. 2015;49(1):237–44.
Nikolaidis P, Dellal A, Torres-Luque G, Ingebrigtsen J. Determinants of acceleration and maximum speed phase of repeated sprint ability in soccer players: a cross-sectional study. Sci Sports. 2015;30(1):e7–16.
Padulo J, Ardigo L, Attene G, Cava C, Wong D, Chamari K, et al. The effect of slope on repeated sprint ability in young soccer players. Res Sports Med. 2016;24(4):320–30.
Padulo J, Di Giminiani R, Ibba G, Zarrouk N, Moalla W, Attene G, et al. The acute effect of whole body vibration on repeated shuttle-running in young soccer players. Int J Sports Med. 2014;35(01):49–54.
Petisco C, Ramirez-Campillo R, Hernández D, Gonzalo-Skok O, Nakamura FY, Sanchez-Sanchez J. Post-activation potentiation: effects of different conditioning intensities on measures of physical fitness in male young professional soccer players. Front Physiol. 2019;10(JUN).
Purkhús E, Krustrup P, Mohr M. High-intensity training improves exercise performance in elite women volleyball players during a competitive season. J Strength Cond Res. 2016;30(11):3066–72.
Pyne DB, Saunders PU, Montgomery PG, Hewitt AJ, Sheehan K. Relationships between repeated sprint testing, speed, and endurance. J Strength Cond Res. 2008;22(5):1633–7.
Ramírez-Campillo R, González-Jurado JA, Martínez C, Nakamura FY, Peñailillo L, Meylan CMP, et al. Effects of plyometric training and creatine supplementation on maximal-intensity exercise and endurance in female soccer players. J Sci Med Sport. 2016;19(8):682–7.
Rampinini E, Bishop D, Marcora SM, Ferrari Bravo D, Sassi R, Impellizzeri FM. Validity of simple field tests as indicators of match-related physical performance in top-level professional soccer players. Int J Sports Med. 2007;28(3):228–35.
Rey E, Padrón-Cabo A, Fernández-Penedo D. Effects of sprint training with and without weighted vest on speed and repeated sprint ability in male soccer players. J Strength Cond Res. 2017;31(10):2659–66.
Rodríguez-Fernández A, Rodríguez-Marroyo J, Casamichana D, Villa J. Effects of 5-week pre-season small-sided-game-based training on repeat sprint ability. J Sports Med Phys Fit. 2016;57(5):529–36.
Røksund OD, Kristoffersen M, Bogen BE, Wisnes A, Engeseth MS, Nilsen AK, et al. Higher drop in speed during a repeated sprint test in soccer players reporting former hamstring strain injury. Front Physiol. 2017;8.
Ruscello B, Esposito M, Partipilo F, Di Cicco D, Filetti C, Pantanella L, et al. Exercise-to-rest ratios in repeated sprint ability training in women’s soccer. J Sports Med Phys Fit. 2017;58(12):1790–9.
Salleh OM, Nadzalan AM, Mohamad NI, Rahmat A. Repeated sprint ability depending on the level of condition among university soccer players. Int J Acad Res Bus Soc Sci. 2017;7(6):506–14.
Sánchez-Sánchez J, García-Unanue J, Hernando E, López-Fernández J, Colino E, León-Jiménez M, et al. Repeated sprint ability and muscular responses according to the age category in elite youth soccer players. Front Physiol. 2019;10.
Sanchez-Sanchez J, Rodriguez A, Petisco C, Ramirez-Campillo R, Martínez C, Nakamura FY. Effects of different post-activation potentiation warm-ups on repeated sprint ability in soccer players from different competitive levels. J Hum Kinet. 2018;61(1):189–97.
Sanders GJ, Turner Z, Boos B, Peacock CA, Peveler W, Lipping A. Aerobic capacity is related to repeated sprint ability with sprint distances less than 40 meters. Int J Exerc Sci. 2017;10(2):197.
Scanlan AT, Madueno MC. Passive recovery promotes superior performance and reduced physiological stress across different phases of short-distance repeated sprints. J Strength Cond Res. 2016;30(9):2540–9.
Scanlan AT, Madueno MC, Guy JH, Giamarelos K, Spiteri T, Dalbo VJ. Measuring decrement in change-of-direction speed across repeated sprints in basketball: novel vs. traditional approaches. J Strength Cond Res. 2021;35(3):841–5.
Selmi W, Rebai H, Chtara M, Naceur A, Sahli S. Self-confidence and affect responses to short-term sprint interval training. Physiol Behav. 2018;188:42–7.
Shalfawi SAI, Enoksen E, Tønnessen E. The relationship between measures of sprinting, aerobic fitness, and lower body strength and power in well-trained female soccer players. Int J Appl Sports Sci. 2014;26(1):18–25.
Shalfawi SA, Ingebrigtsen J, Dillern T, Tønnessen E, Delp TK, Enoksen E. The effect of 40 m repeated sprint training on physical performance in young elite male soccer players. Serb J Sports Sci. 2012;6(3):111–6.
Shalfawi SA, Young M, Tønnessen E, Haugen TA, Enoksen E. The effect of repeated agility training vs. repeated sprint training on elite female soccer players' physical performance. Kinesiol Slov. 2013;19(3).
Silva RLC, Hall E, Maior AS. Inspiratory muscle training improves performance of a repeated sprints ability test in professional soccer players. J Bodywork Mov Ther. 2019;23(3):452–5.
Soares-Caldeira LF, de Souza EA, de Freitas VH, de Moraes SM, Leicht AS, Nakamura FY. Effects of additional repeated sprint training during preseason on performance, heart rate variability, and stress symptoms in futsal players: a randomized controlled trial. J Strength Cond Res. 2014;28(10):2815–26.
Spineti J, Figueiredo T, Assis M, Miranda H, Simão R. Comparison between traditional strength training and complex contrast training on repeated sprint ability and muscle architecture in elite soccer players. J Sports Med Phys Fit. 2015;56(11):1269–78.
Stojanovic M, Ostojic S, Calleja-González J, Milosevic Z, Mikic M. Correlation between explosive strength, aerobic power and repeated sprint ability in elite basketball players. J Sports Med Phys Fit. 2012;52(4):375.
Teixeira AS, Arins FB, De Lucas RD, Carminatti LJ, Dittrich N, Nakamura FY, et al. Comparative effects of two interval shuttle-run training modes on physiological and performance adaptations in female professional futsal players. J Strength Cond Res. 2019;33(5):1416–28.
Thomassen M, Christensen PM, Gunnarsson TP, Nybo L, Bangsbo J. Effect of 2-wk intensified training and inactivity on muscle Na+–K+ pump expression, phospholemman (FXYD1) phosphorylation, and performance in soccer players. J Appl Physiol. 2010;108(4):898–905.
Tønnessen E, Shalfawi SA, Haugen T, Enoksen E. The effect of 40-m repeated sprint training on maximum sprinting speed, repeated sprint speed endurance, vertical jump, and aerobic capacity in young elite male soccer players. J Strength Cond Res. 2011;25(9):2364–70.
Torreblanca-Martinez V, Nevado-Garrosa F, Otero-Saborido FM, Gonzalez-Jurado JA. Effects of fatigue induced by repeated-sprint on kicking accuracy and velocity in female soccer players. PLoS One. 2020;15(1).
Trecroci A, Porcelli S, Perri E, Pedrali M, Rasica L, Alberti G, et al. Effects of different training interventions on the recovery of physical and neuromuscular performance after a soccer match. J Strength Cond Res. 2020;34(8):2189–96.
van den Tillaar R. Comparison of step-by-step kinematics in repeated 30-m sprints in female soccer players. J Strength Cond Res. 2018;32(7):1923–8.
Vasquez-Bonilla AA, Camacho-Cardeñosa A, Timón R, Martínez-Guardado I, Camacho-Cardeñosa M, Olcina G. Muscle oxygen desaturation and re-saturation capacity limits in repeated sprint ability performance in women soccer players: a new physiological interpretation. Int J Environ Res. 2021;18(7):3484.
Wadley G, Le Rossignol P. The relationship between repeated sprint ability and the aerobic and anaerobic energy systems. J Sci Med Sport. 1998;1(2):100–10.
West DJ, Russell M, Bracken RM, Cook CJ, Giroud T, Kilduff LP. Post-warmup strategies to maintain body temperature and physical performance in professional rugby union players. J Sports Sci. 2016;34(2):110–5.
Yanci J, Castillo D, Iturricastillo A, Ayarra R, Nakamura FY. Effects of two different volume-equated weekly distributed short-term plyometric training programs on futsal players’ physical performance. J Strength Cond Res. 2017;31(7):1787–94.
Zagatto AM, Dutra YM, Claus G, de Sousa ME, de Poli RAB, Brisola GMP, et al. Drop jumps improve repeated sprint ability performances in professional basketball players. Biol Sport. 2021;38(4):59–66.
Rampinini E, Bishop D, Marcora S, Bravo DF, Sassi R, Impellizzeri F. Validity of simple field tests as indicators of match-related physical performance in top-level professional soccer players. Int J Sports Med. 2007;28(03):228–35.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Conflict of Interest
All authors declare that they have no conflict of interests relevant to the content of this review.
Data Availability
All data and material reported in this systematic review and meta-analyses are from peer-reviewed publications. All extracted data is available in Supplementary Tables S2 and S3.
Author Contributions
Fraser Thurlow, Jonathon Weakley, Matthew Morrison and Shaun McLaren conceptualised the review and criteria. Fraser Thurlow, Jonathon Weakley, Matthew Morrison and Shaun McLaren completed the screening, data extraction and data analysis of all data within this manuscript. All authors created the tables and figures. All authors contributed to the writing of the manuscript. All authors reviewed, refined and approved the final manuscript.
Additional information
Study Registration
Open Science Framework. Registration https://doi.org/10.17605/OSF.IO/2XQ3A
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thurlow, F., Weakley, J., Townshend, A.D. et al. The Acute Demands of Repeated-Sprint Training on Physiological, Neuromuscular, Perceptual and Performance Outcomes in Team Sport Athletes: A Systematic Review and Meta-analysis. Sports Med 53, 1609–1640 (2023). https://doi.org/10.1007/s40279-023-01853-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-023-01853-w