Abstract
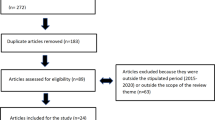
This study evaluated the timing, use, and clinical outcomes of the GeneFolio® Pharmacogenomic Panel in a healthcare setting with patients managed by primary care providers or by psychiatrists. Participants were randomized to receive a pharmacogenetics report at four weeks or 12 weeks. After DNA collection and genetic analysis, pharmacists produced a recommendation report which was given to providers at the randomization week. The four-week group decreased depression severity (PHQ-9 and BDI) faster than the 12-week group (p = 0.0196), and psychiatrists’ patients decreased their depression severity faster than primary care patients (PHQ-9 p = 0.0005, BDI p = 0.0218). Mean mental quality of life increased over time (p < 0.0001), but it increased slower for patients taking drugs in the Significant drug-drug-gene interaction category (p = 0.0012). Mental quality of life, depression severity, and clinical outcomes were improved by GeneFolio® pharmacogenomic testing regardless of provider type, with earlier testing improving outcomes sooner.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data is available from the corresponding author upon reasonable request.
References
Czeisler MÉLR, Petrosky E, Wiley JF, Christensen A, Njai R, et al. (June 24–30, 2020). Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic—United States: MMWR Morb Mortal Wkly Rep.
World Health Organization. Mental Health: Illness and Wellness (2017/090). J Midwifery Women’s Health. 2017;62:767–8.
National Institute of Mental Health (2017). Major Depression Statitistics: https://www.nimh.nih.gov/health/statistics/major-depression.shtml.
Pratt LA, Brody DJ, Gu Q. Antidepressant use among persons aged 12 and over: United States, 2011–2014. NCHS Data Brief 2017: 1–8.
Gibson TB, Jing Y, Smith Carls G, Kim E, Bagalman JE, Burton WN, et al. Cost burden of treatment resistance in patients with depression. Am J Manag Care. 2010;16:370–7.
Glassman AH, Shapiro PA. Depression and the course of coronary artery disease. Am J Psychiatry. 1998;155:4–11.
de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosom Med. 2001;63:619–30.
Kane S (2019). The Top 200 of 2019, ClinCalc DrugStats Database, Version 19.1. In: MEPS prescribed medicines file: ClinCalc: https://clincalc.com/DrugStats/Top200Drugs.aspx.
CDC (2017). Therapeutic Drug Use. In: National Center for Health Statistics. Center for Disease Control: CDC/National Center for Health Statistics.
Beardsley RS, Gardocki GJ, Larson DB, Hidalgo J. Prescribing of psychotropic medication by primary care physicians and psychiatrists. Arch Gen Psychiatry. 1988;45:1117–9.
Haftgoli N, Favrat B, Verdon F, Vaucher P, Bischoff T, Burnand B, et al. Patients presenting with somatic complaints in general practice: depression, anxiety and somatoform disorders are frequent and associated with psychosocial stressors. BMC Fam Pr. 2010;11:67.
Walsh M, Duffy I. A descriptive study of antidepressant prescribing in a semi-rural practice. Ir Med J. 2018;111:752.
Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163:28–40.
Sinyor M, Schaffer A, Levitt A. The sequenced treatment alternatives to relieve depression (STAR*D) trial: a review. Can J Psychiatry. 2010;55:126–35.
Birnbaum HG, Kessler RC, Kelley D, Ben-Hamadi R, Joish VN, Greenberg PE. Employer burden of mild, moderate, and severe major depressive disorder: mental health services utilization and costs, and work performance. Depress Anxiety. 2010;27:78–89.
Fostick L, Silberman A, Beckman M, Spivak B, Amital D. The economic impact of depression: resistance or severity? Eur Neuropsychopharmacol. 2010;20:671–5.
Fagerness J, Fonseca E, Hess GP, Scott R, Gardner KR, Koffler M, et al. Pharmacogenetic-guided psychiatric intervention associated with increased adherence and cost savings. Am J Manag Care. 2014;20:e146–156.
Weitzel KW, Cavallari LH, Lesko LJ. Preemptive panel-based pharmacogenetic testing: the time is now. Pharm Res. 2017;34:1551–5.
Mrazek DA, Biernacka JM, McAlpine DE, Benitez J, Karpyak VM, Williams MD, et al. Treatment outcomes of depression: the pharmacogenomic research network antidepressant medication pharmacogenomic study. J Clin Psychopharmacol. 2014;34:313–7.
Hall-Flavin DK, Winner JG, Allen JD, Carhart JM, Proctor B, Snyder KA, et al. Utility of integrated pharmacogenomic testing to support the treatment of major depressive disorder in a psychiatric outpatient setting. Pharmacogenet Genom. 2013;23:535–48.
Hall-Flavin DK, Winner JG, Allen JD, Jordan JJ, Nesheim RS, Snyder KA, et al. Using a pharmacogenomic algorithm to guide the treatment of depression. Transl Psychiatry. 2012;2:e172.
Winner J, Allen JD, Altar CA, Spahic-Mihajlovic A. Psychiatric pharmacogenomics predicts health resource utilization of outpatients with anxiety and depression. Transl Psychiatry. 2013;3:e242.
Flockhart DA, Skaar T, Berlin DS, Klein TE, Nguyen AT. Clinically available pharmacogenomics tests. Clin Pharmacol Ther. 2009;86:109–13.
Expanding role of pharmacists in adult patients with depression in an outpatient psychiatric clinic to include pharmacogenetic data. Mayo Clinic Individualizing Medicine Conference; Rochester, MN. 2017.
Verbeurgt P, Mamiya T, Oesterheld J. How common are drug and gene interactions? Prevalence in a sample of 1143 patients with CYP2C9, CYP2C19, and CYP2D6 genotyping. Pharmacogenomics. 2014;15:655–65.
Gelenberg AJ, Freeman MP, Markowitz JC, Rosenbaum JF, Thase ME, Trivedi MH (2010). Practice Guideline for the Treatment of Patients wtih Major Depressive Disorder. American Psychiatric Association: https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/mdd.pdf.
Singh AB. Improved antidepressant remission in major depression via a pharmacokinetic pathway polygene pharmacogenetic report. Clin Psychopharmacol Neurosci. 2015;13:150–6.
Altar CA, Carhart J, Allen JD, Hall-Flavin D, Winner J, Dechairo B. Clinical utility of combinatorial pharmacogenomics-guided antidepressant therapy: evidence from three clinical studies. Mol Neuropsychiatry. 2015;1:145–55.
Bradley P, Shiekh M, Mehra V, Vrbicky K, Layle S, Olson MC, et al. Improved efficacy with targeted pharmacogenetic-guided treatment of patients with depression and anxiety: A randomized clinical trial demonstrating clinical utility. J Psychiatr Res. 2018;96:100–7.
Brown-Rice KA, Scholl JL, Fercho KA, Pearson K, Kallsen NA, Davies GE, et al. Neural andcf psychological characteristics of college students with alcoholic parents differ depending on current alcohol use. Prog Neuropsychopharmacol Biol Psychiatry. 2018;81:284–96.
Hocum BT, White JR Jr., Heck JW, Thirumaran RK, Moyer N, Newman R, et al. Cytochrome P-450 gene and drug interaction analysis in patients referred for pharmacogenetic testing. Am J Health-Syst Pharm: AJHP: Off J Am Soc Health-Syst Pharmacists. 2016;73:61–7.
Ware J, Kosinski M, Keller S. SF-36 physical and mental health summary scales. A User’s Manual 2001; 1994.
Steiner AJ, Recacho J, Vanle B, Dang J, Wright SM, Miller JS, et al. Quality of life, functioning, and depressive symptom severity in older adults with major depressive disorder treated with Citalopram in the STAR*D Study. J Clin Psychiatry. 2017;78:897–903.
Acknowledgements
We would like to acknowledge the Avera Institute for Human Genetics laboratory and clinical staff, the Avera Medical Group Clinics and University Psychiatry Associates, Matthew Stanley, DO, Shawn VanGerpen, MD, Timothy Soundy, MD, and the University of South Dakota Sanford School of Medicine Department of Psychiatry Residency Program.
Author information
Authors and Affiliations
Contributions
KB was responsible for study design, protocol, provider education, interpreting results, and the final manuscript. JK was responsible for study design, protocol, patient screening and enrollment, data extraction, interpreting results, and the manuscript. MN was responsible for interpreting the results through the statistical analysis, and contributed tables, descriptions, and revisions to the manuscript. LW and NM were integrally involved in the study through pharmacist report creation, data collection, and analysis, and contributed to the manuscript. JF was involved in the study protocol, patient enrollment, study coordination, and reviewing the manuscript. NB and LC acquired data, were involved in interpreting results, and provided manuscript revisions. GD was involved in overall design of the study and reviewed the manuscript. EE was involved in interpreting results, updating the reference list, and provided manuscript revisions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bohlen, K.N., Kittelsrud, J.M., Nelson, M.E. et al. Clinical utility of pharmacogenetics in a psychiatric and primary care population. Pharmacogenomics J 23, 21–27 (2023). https://doi.org/10.1038/s41397-022-00292-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41397-022-00292-6