Abstract
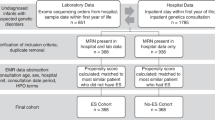
There is an increasing demand for supporting the adoption of rapid whole-genome sequencing (rWGS) by demonstrating its real-world value. We aimed to assess the cost-effectiveness of rWGS in critically ill pediatric patients with diseases of unknown cause. Data were collected prospectively of patients admitted to the Nicklaus Children’s Hospital’s intensive care units from March 2018 to September 2020, with rWGS (N = 65). Comparative data were collected in a matched retrospective cohort with standard diagnostic genetic testing. We determined total costs, diagnostic yield (DY), and incremental cost-effectiveness ratio (ICER) adjusted for selection bias and right censoring. Sensitivity analyses explored the robustness of ICER through bootstrapping. rWGS resulted in a diagnosis in 39.8% while standard testing in 13.5% (p = 0.026). rWGS resulted in a mean saving per person of $100,440 (SE = 26,497, p < 0.001) and a total of $6.53 M for 65 patients. rWGS in critically ill pediatric patients is cost-effective, cost-saving, shortens diagnostic odyssey, and triples the DY of traditional approaches.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others

Data availability
The data that support the findings of this study are available from Nicklaus’ Children hospital, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Nicklaus’ Children hospital.
Code availability
The STATA codes used in this study are available from the authors upon request.
References
Ontario Health (Quality). Genome-wide sequencing for unexplained developmental disabilities or multiple congenital anomalies: a health technology assessment. Ont Health Technol Assess Ser. 2020;20:1–178.
Lionel AC, Costain G, Monfared N, Walker S, Reuter MS, Hosseini SM, et al. Improved diagnostic yield compared with targeted gene sequencing panels suggests a role for whole-genome sequencing as a first-tier genetic test. Genet Med. 2018;20:435–43. https://doi.org/10.1038/gim.2017.119.
Friedman JM, Bombard Y, Cornel MC, Fernandez CV, Junker AK, Plon SE, et al. Genome-wide sequencing in acutely ill infants: genomic medicine’s critical application? Genet Med. 2019;21:498–504. https://doi.org/10.1038/s41436-018-0055-z.
Alam K, Schofield D. Economic evaluation of genomic sequencing in the paediatric population: a critical review. Eur J Hum Genet. 2018;26:1241–7. https://doi.org/10.1038/s41431-018-0175-6.
Farnaes L, Hildreth A, Sweeney NM, Clark MM, Chowdhury S, Nahas S, et al. Rapid whole-genome sequencing decreases infant morbidity and cost of hospitalization. npj Genom Med. 2018;3:10. https://doi.org/10.1038/s41525-018-0049-4.
Rare Diseases Europe. What is a rare disease? Eurordis-Rare Diseases. Survey of the delay in diagnosis for 8 rare diseases In Europe (‘EURORDISCARE 2’) diseases and countries number of respondents by country. Europe. www.Eurodis.org. Accessed 27 April 2021.
Shashi V, McConkie-Rosell A, Rosell B, Schoch K, Vellore K, McDonald M, et al. The utility of the traditional medical genetics diagnostic evaluation in the context of next-generation sequencing for undiagnosed genetic disorders. Genet Med. 2014;16:176–82. https://doi.org/10.1038/gim.2013.99.
Bloss CS, Zeeland AASV, Topol SE, Darst BF, Boeldt DL, Erikson GA, et al. A genome sequencing program for novel undiagnosed diseases. Genet Med. 2015;17:995–1001. https://doi.org/10.1038/gim.2015.21.
Sanford EF, Clark MM, Farnaes L, Williams MR, Perry JC, Ingulli EG, et al. Rapid whole genome sequencing has clinical utility in children in the PICU*. Pediatr Crit Care Med. 2019;20:1007–20. https://doi.org/10.1097/PCC.0000000000002056.
Willig LK, Petrikin JE, Smith LD, Saunders CJ, Thiffault I, Miller NA, et al. Whole-genome sequencing for identification of Mendelian disorders in critically ill infants: a retrospective analysis of diagnostic and clinical findings. Lancet Respir Med. 2015;3:377–87. https://doi.org/10.1016/S2213-2600(15)00139-3.
Dimmock DP, Clark MM, Gaughran M, Cakici JA, Caylor SA, Clarke C, et al. An RCT of rapid genomic sequencing among seriously ill infants results in high clinical utility, changes in management, and low perceived harm. Am J Hum Genet. 2020;107:942–52. https://doi.org/10.1016/j.ajhg.2020.10.003.
Soden SE, Saunders CJ, Willig LK, Farrow EG, Smith LD, Petrikin JE, et al. Effectiveness of exome and genome sequencing guided by acuity of illness for diagnosis of neurodevelopmental disorders. Sci Transl Med. 2014;6:265ra168–265ra168. https://doi.org/10.1126/scitranslmed.3010076.
Dimmock D, Caylor S, Waldman B, Benson W, Ashburner C, Carmichael JL, et al. Project Baby Bear: Rapid precision care incorporating rWGS in 5 California children’s hospitals demonstrates improved clinical outcomes and reduced costs of care. Am J Hum Genet. 2021;108:1231–8. https://doi.org/10.1016/j.ajhg.2021.05.008.
Global. Whole exome and whole genome sequencing. 2021. https://static.cigna.com/assets/chcp/pdf/coveragePolicies/medical/mm_Future/mm_0519_coveragepositioncriteria_exome_genome_sequence.pdf. Accessed 27 April 2021.
Aetna. Subject: genetic testing. 2021. http://www.aetna.com/cpb/medical/data/100_199/0140.html. Accessed 27 April 2021.
UnitedHealthcare. Whole exome and whole genome sequencing UnitedHealthcare ® commercial medical policy whole exome and whole genome sequencing. 2021. https://www.uhcprovider.com/content/dam/provider/docs/public/policies/comm-medical-drug/whole-exome-and-whole-genome-sequencing.pdf.
Genetic Testing - Medical Clinical Policy Bulletins | Aetna. http://www.aetna.com/cpb/medical/data/100_199/0140.html.
Personalized Medicine Coalition - Advocates for precision medicine: understanding genomic testing utilization and coverage in the US. http://www.personalizedmedicinecoalition.org/Resources/Understanding_Genomic_Testing_Utilization_and_Coverage_in_the_US. Accessed 27 April 2021.
Sabatini LM, Mathews C, Ptak D, Doshi S, Tynan K, Hegde MR, et al. Genomic sequencing procedure microcosting analysis and health economic cost-impact analysis. J Mol Diagnostics. 2016;18:319–28. https://doi.org/10.1016/j.jmoldx.2015.11.010.
Dewey FE, Grove ME, Pan C, Goldstein BA, Bernstein JA, Chaib H, et al. Clinical interpretation and implications of whole-genome sequencing. JAMA. 2014;311:1035. https://doi.org/10.1001/jama.2014.1717.
Febres-Aldana CA, Pelaez L, Wright MS, Maher OM, Febres-Aldana AJ, Sasaki J, et al. A case of UDP-galactose 4′-epimerase deficiency associated with dyshematopoiesis and atrioventricular valve malformations: an exceptional clinical phenotype explained by altered n-glycosylation with relative preservation of the leloir pathway. Mol Syndromol. 2020;11:320–30. https://doi.org/10.1159/000511343.
Elixhauser Comorbidity Software, Version 3.7. https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp. Accessed 27 April 2021.
Thompson NR, Fan Y, Dalton JE, Jehi L, Rosenbaum BP, Vadera S, et al. A new Elixhauser-based comorbidity summary measure to predict in-hospital mortality. Med Care. 2015;53:374–9. https://doi.org/10.1097/MLR.0000000000000326.
Sekhon J. The Neyman-Rubin Model of Causal Inference and Estimation via Matching Methods. Box-Steffensmeier J, Brady H, Collier D, eds Oxford Handbook of Political Methodology Oxford Oxford University Press. 2009. https://www.oxfordhandbooks.com/view/10.1093/oxfordhb/9780199286546.001.0001/oxfordhb-9780199286546-e-11.
Li X, Shen C. Doubly robust estimation of causal effect. Circ Cardiovasc Qual Outcomes. 2020;13:e006065. https://doi.org/10.1161/CIRCOUTCOMES.119.006065.
Rosenbaum PR. Model-based direct adjustment. J Am Stat Assoc. 1987;82:387–94. https://doi.org/10.2307/2289440.
Robins JM, Rotnitzky A, Zhao LP. Estimation of regression coefficients when some regressors are not always observed. J Am Stat Assoc. 1994;89:846–66. https://doi.org/10.1080/01621459.1994.10476818.
Scharfstein DO, Rotnitzky A, Robins JM. Adjusting for nonignorable drop-out using semiparametric nonresponse models. J Am Stat Assoc. 1999;94:1096–120. https://doi.org/10.1080/01621459.1999.10473862.
Bang H, Robins JM. Doubly robust estimation in missing data and causal inference models. Biometrics. 2005;61:962–73. https://doi.org/10.1111/j.1541-0420.2005.00377.x.
Robins J, Sued M, Lei-Gomez Q, Rotnitzky A. Comment: performance of double-robust estimators when “inverse probability” weights are highly variable. Stat Sci. 2007;22:544–59. https://doi.org/10.1214/07-STS227D.
Li J, Vachani A, Epstein A, Mitra N. A doubly robust approach for cost-effectiveness estimation from observational data. Stat Methods Med Res. 2018;27:3126–38. https://doi.org/10.1177/0962280217693262.
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47:626–33. https://doi.org/10.1097/MLR.0b013e31819432e5.
Sun JW, Bourgeois FT, Haneuse S, Hernández-Díaz S, Landon JE, Bateman BT, et al. Development and validation of a pediatric comorbidity index. Am J Epidemiol. 2021;190:918–27. https://doi.org/10.1093/aje/kwaa244.
Petrikin JE, Cakici JA, Clark MM, Willig LK, Sweeney NM, Farrow EG, et al. The NSIGHT1-randomized controlled trial: rapid whole-genome sequencing for accelerated etiologic diagnosis in critically ill infants. NPJ Genom Med. 2018;3:6 https://doi.org/10.1038/s41525-018-0045-8.
Diagnosis Related Group (DRG). https://hmsa.com/portal/provider/zav_pel.fh.DIA.650.htm. Accessed 27 April 2021.
Krantz ID, Medne L, Weatherly JM, Wild KT, Biswas S, Devkota B, et al. Effect of whole-genome sequencing on the clinical management of acutely ill infants with suspected genetic disease: a randomized clinical trial. JAMA Pediatr. 2021;175:1218–26. https://doi.org/10.1001/jamapediatrics.2021.3496.
Kingsmore SF, Cakici JA, Clark MM, Gaughran M, Feddock M, Batalov S, et al. A randomized, controlled trial of the analytic and diagnostic performance of singleton and trio, rapid genome and exome sequencing in ill infants. Am J Hum Genet. 2019;105:719–33. https://doi.org/10.1016/j.ajhg.2019.08.009.
Dragojlovic N, Elliott AM, Adam S, van Karnebeek C, Lehman A, Mwenifumbo JC, et al. The cost and diagnostic yield of exome sequencing for children with suspected genetic disorders: a benchmarking study. Genet Med. 2018;20:1013–21. https://doi.org/10.1038/gim.2017.226.
Ellsworth KA, Caylor S, Benson W, Ashburner C, Carmichael J, Cham E, et al. Abstracts from the 53rd European Society of Human Genetics (ESHG) Conference: Oral Presentations. Eur J Hum Genet. 2020;28:1–140. https://doi.org/10.1038/s41431-020-00740-6.
Project Baby Bear Final Report; 2020. https://radygenomics.org/wp-content/uploads/2020/07/PBB-Final-Report_07.14.20.pdf.
Smith HS, Swint JM, Lalani SR, de Oliveira Otto MC, Yamal JM, Russell HV, et al. Exome sequencing compared with standard genetic tests for critically ill infants with suspected genetic conditions. Genet Med. 2020;22:1303–10. https://doi.org/10.1038/s41436-020-0798-1.
Acknowledgements
We would like to acknowledge Rene Medina for their contribution to the data extraction and Jennifer McCafferty for assistance in Baby Manatee program development.
Funding
This study was supported by Florida Department of Heath State Appropriation, Cornelia T. Bailey Foundation, Sanford Health and Nicklaus Children’s Health Care Foundation.
Author information
Authors and Affiliations
Contributions
Conceptualization: VD, DS2. Data curation: PE, MJ, DS, AG, PJ, MDB, BT, JS, AJ, DS2. Formal Analysis: VD, AB, YH, RM, PE, MJ, DS, AG, DS2. Funding Acquisition: VD, DS2. Investigation: PE, MJ, DS, AG, PJ, MDB, BT, JS, AJ, DS2. Methodology: VD, AB, YH, PE, AG, PJ, MDB, BT, JS, AJ, DS2. Project administration: PE, MJ, DS, DS2. Resource: PE, PJ, MDB, BT, JS, AJ. Supervision: VD, PE, DS2. Validation: PE, MJ, DS, AG, PJ, MDB, BT, JS, AJ, DS2. Writing – original draft: VD, AB, YH, DS, PE, AG, DS2. Writing – review & editing: VD, AB, YH, DS, PE, AG, PJ, MDB, BT, JS, AJ, DS2. (DS = Diana Soler, DS2 = Daria Salyakina).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The data used for analyses within the project were de-identified.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Diaby, V., Babcock, A., Huang, Y. et al. Real-world economic evaluation of prospective rapid whole-genome sequencing compared to a matched retrospective cohort of critically ill pediatric patients in the United States. Pharmacogenomics J 22, 223–229 (2022). https://doi.org/10.1038/s41397-022-00277-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41397-022-00277-5
This article is cited by
-
Rapid genomic sequencing for genetic disease diagnosis and therapy in intensive care units: a review
npj Genomic Medicine (2024)
-
Genomic medicine in neonatal care: progress and challenges
European Journal of Human Genetics (2023)
-
Role of genomic medicine and implementing equitable access for critically ill infants in neonatal intensive care units
Journal of Perinatology (2023)
-
Resource allocation in genetic and genomic medicine
Journal of Community Genetics (2022)