当前位置:
X-MOL 学术
›
Theranostics
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
MRI and histological evaluation of pulsed focused ultrasound and microbubbles treatment effects in the brain.
Theranostics ( IF 12.4 ) Pub Date : 2018-09-09 , DOI: 10.7150/thno.24512 Zsofia I Kovacs 1 , Tsang-Wei Tu 1, 2, 3 , Maggie Sundby 1 , Farhan Qureshi 1 , Bobbi K Lewis 1 , Neekita Jikaria 1 , Scott R Burks 1 , Joseph A Frank 1, 4
Theranostics ( IF 12.4 ) Pub Date : 2018-09-09 , DOI: 10.7150/thno.24512 Zsofia I Kovacs 1 , Tsang-Wei Tu 1, 2, 3 , Maggie Sundby 1 , Farhan Qureshi 1 , Bobbi K Lewis 1 , Neekita Jikaria 1 , Scott R Burks 1 , Joseph A Frank 1, 4
Affiliation
|
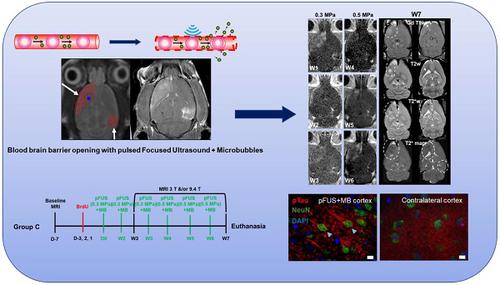
Magnetic resonance imaging (MRI)-guided pulsed focused ultrasound (pFUS) combined with microbubbles (MB) contrast agent infusion has been shown to transiently disrupt the blood-brain barrier (BBBD), increasing the delivery of neurotherapeutics to treat central nervous system (CNS) diseases. pFUS interaction with the intravascular MB results in acoustic cavitation forces passing through the neurovascular unit (NVU), inducing BBBD detected on contrast-enhanced MRI. Multiple pFUS+MB exposures in Alzheimer's disease (AD) models are being investigated as a method to clear amyloid plaques by activated microglia or infiltrating immune cells. Since it has been reported that pFUS+MB can induce a sterile inflammatory response (SIR) [1-5] in the rat, the goal of this study was to investigate the potential long-term effects of SIR in the brain following single and six weekly sonications by serial high-resolution MRI and pathology. Methods: Female Sprague Dawley rats weighing 217±16.6 g prior to sonication received bromo-deoxyuridine (BrdU) to tag proliferating cells in the brain. pFUS was performed at 548 kHz, ultrasound burst 10 ms and initial peak negative pressure of 0.3 MPa (in water) for 120 s coupled with a slow infusion of ~460 µL/kg (5-8×107 MB) that started 30 s before and 30 s during sonication. Nine 2 mm focal regions in the left cortex and four regions over the right hippocampus were treated with pFUS+MB. Serial high-resolution brain MRIs at 3 T and 9.4 T were obtained following a single or during the course of six weekly pFUS+MB resulting in BBBD in the left cortex and the right hippocampus. Animals were monitored over 7 to 13 weeks and imaging results were compared to histology. Results: Fewer than half of the rats receiving a single pFUS+MB exposure displayed hypointense voxels on T2*-weighted (w) MRI at week 7 or 13 in the cortex or hippocampus without differences compared to the contralateral side on histograms of T2* maps. Single sonicated rats had evidence of limited microglia activation on pathology compared to the contralateral hemisphere. Six weekly pFUS+MB treatments resulted in pathological changes on T2*w images with multiple hypointense regions, cortical atrophy, along with 50% of rats having persistent BBBD and astrogliosis by MRI. Pathologic analysis of the multiple sonicated animals demonstrated the presence of metallophagocytic Prussian blue-positive cells in the parenchyma with significantly (p<0.05) increased areas of activated astrocytes and microglia, and high numbers of systemic infiltrating CD68+ macrophages along with BrdU+ cells compared to contralateral brain. In addition, multiple treatments caused an increase in the number of hyperphosphorylated Tau (pTau)-positive neurons containing neurofibrillary tangles (NFT) in the sonicated cortex but not in the hippocampus when compared to contralateral brain, which was confirmed by Western blot (WB) (p<0.04). Conclusions: The repeated SIR following multiple pFUS+MB treatments could contribute to changes on MR imaging including persistent BBBD, cortical atrophy, and hypointense voxels on T2w and T2*w images consistent with pathological injury. Moreover, areas of astrogliosis, activated microglia, along with higher numbers of CD68+ infiltrating macrophages and BrdU+ cells were detected in multiple sonicated areas of the cortex and hippocampus. Elevations in pTau and NFT were detected in neurons of the multiple sonicated cortex. Minimal changes on MRI and histology were observed in single pFUS+MB-treated rats at 7 and 13 weeks post sonication. In comparison, animals that received 6 weekly sonications demonstrated evidence on MRI and histology of vascular damage, inflammation and neurodegeneration associated with the NVU commonly observed in trauma. Further investigation is recommended of the long-term effects of multiple pFUS+MB in clinical trials.
中文翻译:

脉冲聚焦超声和微泡对大脑的治疗的MRI和组织学评估。
磁共振成像(MRI)引导的脉冲聚焦超声(pFUS)结合微泡(MB)造影剂输注已显示出暂时破坏血脑屏障(BBBD),从而增加了神经疗法治疗中枢神经系统(CNS)的能力)疾病。pFUS与血管内MB的相互作用导致声空化力通过神经血管单位(NVU),从而诱发在对比增强MRI上检测到的BBBD。正在研究在阿尔茨海默氏病(AD)模型中多次暴露于pFUS + MB,作为通过活化的小胶质细胞或浸润的免疫细胞清除淀粉样蛋白斑块的方法。由于据报道pFUS + MB可以在大鼠中诱发无菌性炎症反应(SIR)[1-5],这项研究的目的是通过连续高分辨率MRI和病理学研究单次和每周6次超声后SIR对大脑的潜在长期影响。方法:超声前体重217±16.6 g的雌性Sprague Dawley大鼠接受溴脱氧尿苷(BrdU)标记大脑中的增殖细胞。在548 kHz频率下执行pFUS,超声猝发10 ms,初始峰值负压0.3 MPa(在水中)持续120 s,并在30 s之前开始缓慢注入〜460 µL / kg(5-8×107 MB)超声处理30秒。用pFUS + MB治疗左侧皮质的9个2 mm聚焦区域和右侧海马的4个区域。在3 T和9时进行的连续高分辨率脑MRI。一次或在每周六次pFUS + MB过程中获得4 T,导致左皮质和右海马体中出现BBBD。在7至13周内对动物进行监测,并将成像结果与组织学进行比较。结果:少于一半的接受单次pFUS + MB暴露的大鼠在第7或13周在皮质或海马体的T2 *加权(w)MRI上显示低体素,与T2 *直方图的对侧相比无差异。与对侧半球相比,单只超声处理的大鼠在病理学上具有有限的小胶质细胞激活的证据。每周六次pFUS + MB治疗导致T2 * w图像出现病理变化,出现多个低眼点区域,皮质萎缩,以及50%患有BBBD和星形胶质增生的大鼠(通过MRI)。多个超声处理动物的病理分析表明,实质中存在吞噬细胞的普鲁士蓝阳性细胞,激活星形胶质细胞和小胶质细胞的面积显着增加(p <0.05),并且与对侧相比,大量的全身浸润性CD68 +巨噬细胞以及BrdU +细胞脑。此外,与对侧大脑相比,超声处理后的皮质中海马中不包含神经原纤维缠结(NFT)的高磷酸化Tau(pTau)阳性神经元数量增加,而对侧大脑则证实了这一点。 (p <0.04)。结论:多次pFUS + MB治疗后重复进行SIR可能有助于MR影像学改变,包括持续性BBBD,皮质萎缩,T2w和T2 * w图像上的低水平体素与病理损伤一致。此外,在皮质和海马体的多个超声区域中检测到了星形胶质化,激活的小胶质细胞以及CD68 +浸润性巨噬细胞和BrdU +细胞数量增加的区域。在多个超声皮层的神经元中检测到pTau和NFT升高。在超声处理后7周和13周,在单只pFUS + MB处理的大鼠中观察到MRI和组织学的最小变化。相比之下,每周接受6次超声处理的动物在MRI和组织学上显示出与创伤中常见的NVU相关的血管损伤,炎症和神经退行性变的证据。建议在临床试验中进一步研究多种pFUS + MB的长期作用。在大脑皮层和海马体的多个超声区域中,检测到星形胶质细胞增多症,小胶质细胞活化以及CD68 +浸润性巨噬细胞和BrdU +细胞数量增加。在多个超声皮层的神经元中检测到pTau和NFT升高。在超声处理后7周和13周,在单只pFUS + MB处理的大鼠中观察到MRI和组织学的最小变化。相比之下,每周接受6次超声处理的动物在MRI和组织学上显示出与创伤中常见的NVU相关的血管损伤,炎症和神经退行性变的证据。建议在临床试验中进一步研究多种pFUS + MB的长期作用。在大脑皮层和海马体的多个超声区域中,检测到星形胶质细胞增多症,小胶质细胞活化以及CD68 +浸润性巨噬细胞和BrdU +细胞数量增加。在多个超声皮层的神经元中检测到pTau和NFT升高。在超声处理后7周和13周,在单只pFUS + MB处理的大鼠中观察到MRI和组织学的最小变化。相比之下,每周接受6次超声处理的动物在MRI和组织学上显示出与创伤中常见的NVU相关的血管损伤,炎症和神经退行性变的证据。建议在临床试验中进一步研究多种pFUS + MB的长期作用。在皮质和海马体的多个超声区域中检测到较高的CD68 +浸润巨噬细胞和BrdU +细胞数量。在多个超声皮层的神经元中检测到pTau和NFT升高。在超声处理后7周和13周,在单只pFUS + MB处理的大鼠中观察到MRI和组织学的最小变化。相比之下,每周接受6次超声处理的动物在MRI和组织学上显示出与创伤中常见的NVU相关的血管损伤,炎症和神经退行性变的证据。建议在临床试验中进一步研究多种pFUS + MB的长期作用。在皮质和海马体的多个超声区域中检测到较高的CD68 +浸润巨噬细胞和BrdU +细胞数量。在多个超声皮层的神经元中检测到pTau和NFT升高。在超声处理后第7周和第13周,在单只pFUS + MB处理的大鼠中观察到MRI和组织学的最小变化。相比之下,每周接受6次超声处理的动物在MRI和组织学上显示出与创伤中常见的NVU相关的血管损伤,炎症和神经退行性变的证据。建议在临床试验中进一步研究多种pFUS + MB的长期作用。在超声处理后7周和13周,在单只pFUS + MB处理的大鼠中观察到MRI和组织学的最小变化。相比之下,每周接受6次超声处理的动物在MRI和组织学上显示出与创伤中常见的NVU相关的血管损伤,炎症和神经退行性变的证据。建议在临床试验中进一步研究多种pFUS + MB的长期作用。在超声处理后7周和13周,在单只pFUS + MB处理的大鼠中观察到MRI和组织学的最小变化。相比之下,每周接受6次超声处理的动物在MRI和组织学上显示出与创伤中常见的NVU相关的血管损伤,炎症和神经退行性变的证据。建议在临床试验中进一步研究多种pFUS + MB的长期作用。
更新日期:2018-09-25
中文翻译:

脉冲聚焦超声和微泡对大脑的治疗的MRI和组织学评估。
磁共振成像(MRI)引导的脉冲聚焦超声(pFUS)结合微泡(MB)造影剂输注已显示出暂时破坏血脑屏障(BBBD),从而增加了神经疗法治疗中枢神经系统(CNS)的能力)疾病。pFUS与血管内MB的相互作用导致声空化力通过神经血管单位(NVU),从而诱发在对比增强MRI上检测到的BBBD。正在研究在阿尔茨海默氏病(AD)模型中多次暴露于pFUS + MB,作为通过活化的小胶质细胞或浸润的免疫细胞清除淀粉样蛋白斑块的方法。由于据报道pFUS + MB可以在大鼠中诱发无菌性炎症反应(SIR)[1-5],这项研究的目的是通过连续高分辨率MRI和病理学研究单次和每周6次超声后SIR对大脑的潜在长期影响。方法:超声前体重217±16.6 g的雌性Sprague Dawley大鼠接受溴脱氧尿苷(BrdU)标记大脑中的增殖细胞。在548 kHz频率下执行pFUS,超声猝发10 ms,初始峰值负压0.3 MPa(在水中)持续120 s,并在30 s之前开始缓慢注入〜460 µL / kg(5-8×107 MB)超声处理30秒。用pFUS + MB治疗左侧皮质的9个2 mm聚焦区域和右侧海马的4个区域。在3 T和9时进行的连续高分辨率脑MRI。一次或在每周六次pFUS + MB过程中获得4 T,导致左皮质和右海马体中出现BBBD。在7至13周内对动物进行监测,并将成像结果与组织学进行比较。结果:少于一半的接受单次pFUS + MB暴露的大鼠在第7或13周在皮质或海马体的T2 *加权(w)MRI上显示低体素,与T2 *直方图的对侧相比无差异。与对侧半球相比,单只超声处理的大鼠在病理学上具有有限的小胶质细胞激活的证据。每周六次pFUS + MB治疗导致T2 * w图像出现病理变化,出现多个低眼点区域,皮质萎缩,以及50%患有BBBD和星形胶质增生的大鼠(通过MRI)。多个超声处理动物的病理分析表明,实质中存在吞噬细胞的普鲁士蓝阳性细胞,激活星形胶质细胞和小胶质细胞的面积显着增加(p <0.05),并且与对侧相比,大量的全身浸润性CD68 +巨噬细胞以及BrdU +细胞脑。此外,与对侧大脑相比,超声处理后的皮质中海马中不包含神经原纤维缠结(NFT)的高磷酸化Tau(pTau)阳性神经元数量增加,而对侧大脑则证实了这一点。 (p <0.04)。结论:多次pFUS + MB治疗后重复进行SIR可能有助于MR影像学改变,包括持续性BBBD,皮质萎缩,T2w和T2 * w图像上的低水平体素与病理损伤一致。此外,在皮质和海马体的多个超声区域中检测到了星形胶质化,激活的小胶质细胞以及CD68 +浸润性巨噬细胞和BrdU +细胞数量增加的区域。在多个超声皮层的神经元中检测到pTau和NFT升高。在超声处理后7周和13周,在单只pFUS + MB处理的大鼠中观察到MRI和组织学的最小变化。相比之下,每周接受6次超声处理的动物在MRI和组织学上显示出与创伤中常见的NVU相关的血管损伤,炎症和神经退行性变的证据。建议在临床试验中进一步研究多种pFUS + MB的长期作用。在大脑皮层和海马体的多个超声区域中,检测到星形胶质细胞增多症,小胶质细胞活化以及CD68 +浸润性巨噬细胞和BrdU +细胞数量增加。在多个超声皮层的神经元中检测到pTau和NFT升高。在超声处理后7周和13周,在单只pFUS + MB处理的大鼠中观察到MRI和组织学的最小变化。相比之下,每周接受6次超声处理的动物在MRI和组织学上显示出与创伤中常见的NVU相关的血管损伤,炎症和神经退行性变的证据。建议在临床试验中进一步研究多种pFUS + MB的长期作用。在大脑皮层和海马体的多个超声区域中,检测到星形胶质细胞增多症,小胶质细胞活化以及CD68 +浸润性巨噬细胞和BrdU +细胞数量增加。在多个超声皮层的神经元中检测到pTau和NFT升高。在超声处理后7周和13周,在单只pFUS + MB处理的大鼠中观察到MRI和组织学的最小变化。相比之下,每周接受6次超声处理的动物在MRI和组织学上显示出与创伤中常见的NVU相关的血管损伤,炎症和神经退行性变的证据。建议在临床试验中进一步研究多种pFUS + MB的长期作用。在皮质和海马体的多个超声区域中检测到较高的CD68 +浸润巨噬细胞和BrdU +细胞数量。在多个超声皮层的神经元中检测到pTau和NFT升高。在超声处理后7周和13周,在单只pFUS + MB处理的大鼠中观察到MRI和组织学的最小变化。相比之下,每周接受6次超声处理的动物在MRI和组织学上显示出与创伤中常见的NVU相关的血管损伤,炎症和神经退行性变的证据。建议在临床试验中进一步研究多种pFUS + MB的长期作用。在皮质和海马体的多个超声区域中检测到较高的CD68 +浸润巨噬细胞和BrdU +细胞数量。在多个超声皮层的神经元中检测到pTau和NFT升高。在超声处理后第7周和第13周,在单只pFUS + MB处理的大鼠中观察到MRI和组织学的最小变化。相比之下,每周接受6次超声处理的动物在MRI和组织学上显示出与创伤中常见的NVU相关的血管损伤,炎症和神经退行性变的证据。建议在临床试验中进一步研究多种pFUS + MB的长期作用。在超声处理后7周和13周,在单只pFUS + MB处理的大鼠中观察到MRI和组织学的最小变化。相比之下,每周接受6次超声处理的动物在MRI和组织学上显示出与创伤中常见的NVU相关的血管损伤,炎症和神经退行性变的证据。建议在临床试验中进一步研究多种pFUS + MB的长期作用。在超声处理后7周和13周,在单只pFUS + MB处理的大鼠中观察到MRI和组织学的最小变化。相比之下,每周接受6次超声处理的动物在MRI和组织学上显示出与创伤中常见的NVU相关的血管损伤,炎症和神经退行性变的证据。建议在临床试验中进一步研究多种pFUS + MB的长期作用。



























 京公网安备 11010802027423号
京公网安备 11010802027423号