当前位置:
X-MOL 学术
›
Adv. Healthcare Mater.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Acceleration of Diabetic Wound Regeneration using an In Situ–Formed Stem‐Cell‐Based Skin Substitute
Advanced Healthcare Materials ( IF 10.0 ) Pub Date : 2018-07-13 , DOI: 10.1002/adhm.201800432 Yixiao Dong 1 , Melanie Rodrigues 2 , Sun Hyung Kwon 2 , Xiaolin Li 3 , Sigen A 3 , Elizabeth Anne Brett 2 , Nicola Elvassore 1 , Wenxin Wang 3 , Geoffrey C. Gurtner 2
Advanced Healthcare Materials ( IF 10.0 ) Pub Date : 2018-07-13 , DOI: 10.1002/adhm.201800432 Yixiao Dong 1 , Melanie Rodrigues 2 , Sun Hyung Kwon 2 , Xiaolin Li 3 , Sigen A 3 , Elizabeth Anne Brett 2 , Nicola Elvassore 1 , Wenxin Wang 3 , Geoffrey C. Gurtner 2
Affiliation
|
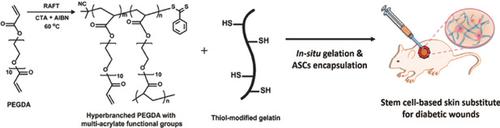
Chronic diabetic ulcers are a common complication in patients with diabetes, often leading to lower limb amputations and even mortality. Stem cells have shown promise in promoting cutaneous wound healing by modulating inflammation, angiogenesis, and re‐epithelialization. However, more effective delivery and engraftment strategies are needed to prolong transplanted stem cell lifespan and their pro‐healing functions in a chronic wound environment to improve skin regeneration. In this study, an injectable poly(ethylene glycol) (PEG)–gelatin‐based hydrogel system is examined to create a functional stem cell niche for the delivery of adipose‐derived stem cells (ASCs) into diabetic wounds. Human ASCs are encapsulated into the in situ crosslinked hydrogels and cultured in a 3D topography. The encapsulated cells are well attached and spread inside the hydrogels, retaining viability, proliferation, and metabolic activity up to three weeks in vitro. Allogeneic ASCs are delivered to diabetic wounds by this hydrogel vehicle. It is found that stem cell retention is significantly improved in vivo with vehicle‐mediated delivery. The ASC‐hydrogel‐based treatment decreases inflammatory cell infiltration, enhances neovascularization, and remarkably accelerates wound closure in diabetic mice. Together, these findings suggest this conveniently‐applicable ASC‐hydrogel‐based skin substitute provides a promising potential for the treatment of chronic diabetic wounds.
中文翻译:

使用原位形成的基于干细胞的皮肤替代物加速糖尿病伤口的再生
慢性糖尿病性溃疡是糖尿病患者的常见并发症,常常导致下肢截肢甚至死亡。干细胞已显示出有望通过调节炎症,血管生成和上皮再生来促进皮肤伤口愈合。但是,需要更有效的递送和植入策略来延长移植的干细胞寿命及其在慢性伤口环境中的修复功能,以改善皮肤再生。在这项研究中,对可注射的聚乙二醇(PEG)-明胶水凝胶系统进行了研究,以创建功能性干细胞生态位,以将脂肪干细胞(ASC)输送至糖尿病伤口。将人类ASC封装在原位交联的水凝胶中,并在3D地形图中进行培养。包封的细胞很好地附着并在水凝胶内散布,在体外最多保持三周的存活率,增殖和代谢活性。该水凝胶媒介物将同种异体ASC递送至糖尿病伤口。发现通过媒介介导的递送在体内显着改善了干细胞的保留。基于ASC水凝胶的治疗减少了炎症细胞浸润,增强了新生血管形成,并显着加速了糖尿病小鼠的伤口闭合。总之,这些发现表明,这种方便实用的基于ASC-水凝胶的皮肤替代品为治疗慢性糖尿病伤口提供了有希望的潜力。发现通过媒介介导的递送在体内显着改善了干细胞的保留。基于ASC水凝胶的治疗减少了炎症细胞浸润,增强了新生血管形成,并显着加速了糖尿病小鼠的伤口闭合。总之,这些发现表明,这种方便实用的基于ASC-水凝胶的皮肤替代品为治疗慢性糖尿病伤口提供了有希望的潜力。发现通过媒介介导的递送在体内显着改善了干细胞的保留。基于ASC水凝胶的治疗减少了炎症细胞浸润,增强了新生血管形成,并显着加速了糖尿病小鼠的伤口闭合。总之,这些发现表明,这种方便实用的基于ASC-水凝胶的皮肤替代品为治疗慢性糖尿病伤口提供了有希望的潜力。
更新日期:2018-07-13
中文翻译:

使用原位形成的基于干细胞的皮肤替代物加速糖尿病伤口的再生
慢性糖尿病性溃疡是糖尿病患者的常见并发症,常常导致下肢截肢甚至死亡。干细胞已显示出有望通过调节炎症,血管生成和上皮再生来促进皮肤伤口愈合。但是,需要更有效的递送和植入策略来延长移植的干细胞寿命及其在慢性伤口环境中的修复功能,以改善皮肤再生。在这项研究中,对可注射的聚乙二醇(PEG)-明胶水凝胶系统进行了研究,以创建功能性干细胞生态位,以将脂肪干细胞(ASC)输送至糖尿病伤口。将人类ASC封装在原位交联的水凝胶中,并在3D地形图中进行培养。包封的细胞很好地附着并在水凝胶内散布,在体外最多保持三周的存活率,增殖和代谢活性。该水凝胶媒介物将同种异体ASC递送至糖尿病伤口。发现通过媒介介导的递送在体内显着改善了干细胞的保留。基于ASC水凝胶的治疗减少了炎症细胞浸润,增强了新生血管形成,并显着加速了糖尿病小鼠的伤口闭合。总之,这些发现表明,这种方便实用的基于ASC-水凝胶的皮肤替代品为治疗慢性糖尿病伤口提供了有希望的潜力。发现通过媒介介导的递送在体内显着改善了干细胞的保留。基于ASC水凝胶的治疗减少了炎症细胞浸润,增强了新生血管形成,并显着加速了糖尿病小鼠的伤口闭合。总之,这些发现表明,这种方便实用的基于ASC-水凝胶的皮肤替代品为治疗慢性糖尿病伤口提供了有希望的潜力。发现通过媒介介导的递送在体内显着改善了干细胞的保留。基于ASC水凝胶的治疗减少了炎症细胞浸润,增强了新生血管形成,并显着加速了糖尿病小鼠的伤口闭合。总之,这些发现表明,这种方便实用的基于ASC-水凝胶的皮肤替代品为治疗慢性糖尿病伤口提供了有希望的潜力。



























 京公网安备 11010802027423号
京公网安备 11010802027423号