当前位置:
X-MOL 学术
›
Acta Biomater.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
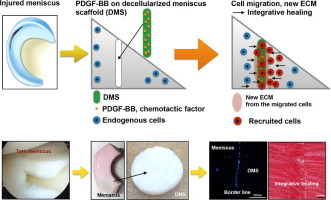
Platelet-derived growth factor-coated decellularized meniscus scaffold for integrative healing of meniscus tears.
Acta Biomaterialia ( IF 9.7 ) Pub Date : 2018-06-14 , DOI: 10.1016/j.actbio.2018.06.021 Kwang Il Lee 1 , Merissa Olmer 1 , Jihye Baek 2 , Darryl D D'Lima 2 , Martin K Lotz 1
Acta Biomaterialia ( IF 9.7 ) Pub Date : 2018-06-14 , DOI: 10.1016/j.actbio.2018.06.021 Kwang Il Lee 1 , Merissa Olmer 1 , Jihye Baek 2 , Darryl D D'Lima 2 , Martin K Lotz 1
Affiliation
|
The aim of this study was to examine the potential of platelet-derived growth factor (PDGF)-coated decellularized meniscus scaffold in mediating integrative healing of meniscus tears by inducing endogenous cell migration. Fresh bovine meniscus was chemically decellularized and covalently conjugated with heparin and PDGF-BB. In vitro PDGF release kinetics was measured. The scaffold was transplanted into experimental tears in avascular bovine meniscus explants and cultured for 2 and 4 weeks. The number migrating and proliferating cells at the borderline between the scaffold and injured explant and PDGF receptor-β (PDGFRβ) expressing cells were counted. The alignment of the newly produced ECM and collagen was analyzed by Safranin-O, picrosirius red staining, and differential interference contrast (DIC). Tensile testing of the explants was performed after culture for 2 and 4 weeks. Heparin conjugated scaffold showed immobilization of high levels of PDGF-BB, with sustained release over 2 weeks. Insertion of the PDGF-BB treated scaffold in defects in avascular meniscus led to increased PDGFRβ expression, cell migration and proliferation into the defect zone. Safranin-O, picrosirius red staining and DIC showed tissue integration between the scaffold and injured explants. Tensile properties of injured explants treated with PDGF-BB coated scaffold were significantly higher than in the scaffold without PDGF. In conclusion, PDGF-BB-coated scaffold increased PDGFRβ expression and promoted migration of endogenous meniscus cells to the defect area. New matrix was formed that bridged the space between the native meniscus and the scaffold and this was associated with improved biomechanical properties. The PDGF-BB-coated scaffold will be promising for clinical translation to healing of meniscus tears.
STATEMENT OF SIGNIFICANCE
Meniscus tears are the most common injury of the knee joint. The most prevalent forms that occur in the inner third typically do not spontaneously heal and represent a major risk factor for the development of knee osteoarthritis. The goal of this project was to develop an approach that is readily applicable for clinical use. We selected a natural and readily available decellularized meniscus scaffold and conjugated it with PDGF, which we had previously found to have strong chemotactic activity for chondrocytes and progenitor cells. The present results show that insertion of the PDGF-conjugated scaffold in defects in avascular meniscus led to endogenous cell migration and proliferation into the defect zone with tissue integration between the scaffold and injured explants and improved tensile properties. This PDGF-conjugated scaffold will be promising for a translational approach to healing of meniscus tears.
中文翻译:

血小板衍生的生长因子包被的脱细胞半月板支架,用于半月板泪液的综合愈合。
这项研究的目的是检查由血小板衍生的生长因子(PDGF)涂层的脱细胞半月板支架在通过诱导内源性细胞迁移介导半月板撕裂的综合愈合中的潜力。将新鲜的牛半月板化学脱细胞并与肝素和PDGF-BB共价缀合。测量了体外PDGF释放动力学。将该支架移植到无血管牛半月板外植体的实验性眼泪中,并培养2周和4周。计算支架和受损外植体之间交界处的迁移和增殖细胞数以及表达PDGF受体-β(PDGFRβ)的细胞。新产生的ECM和胶原蛋白的比对通过番红O型,picrosirius红染色和微分干涉对比(DIC)进行分析。培养2周和4周后,对外植体进行拉伸测试。肝素偶联的支架显示出高水平的PDGF-BB固定化,持续释放超过2周。PDGF-BB处理的支架在无血管半月板缺损处的插入导致PDGFRβ表达增加,细胞迁移以及向缺损区的增殖。番红O-O,picrosirius红染色和DIC显示支架和受伤的外植体之间存在组织整合。用PDGF-BB涂层支架处理的外植体的拉伸特性显着高于未使用PDGF的支架。总之,PDGF-BB涂层的支架增加了PDGFRβ的表达,并促进了内源性半月板细胞向缺损区域的迁移。形成了新的基质,其桥接了天然弯液面和支架之间的空间,这与改善的生物力学性能有关。PDGF-BB涂层支架将有望用于临床修复半月板泪液。意义说明半月板撕裂是膝关节最常见的损伤。发生在内侧三分之一的最普遍的形式通常不会自发愈合,并且是膝盖骨关节炎发展的主要危险因素。该项目的目标是开发一种易于应用于临床的方法。我们选择了一种天然且容易获得的脱细胞半月板支架,并将其与PDGF偶联,我们先前发现PDGF对软骨细胞和祖细胞具有很强的趋化活性。目前的结果表明,PDGF共轭支架在无血管半月板缺陷中的插入导致内源性细胞迁移和扩散进入缺陷区,并在支架和受损外植体之间进行组织整合并改善了拉伸性能。这种PDGF共轭支架将有望用于半月板撕裂愈合的转化方法。
更新日期:2018-06-14
中文翻译:

血小板衍生的生长因子包被的脱细胞半月板支架,用于半月板泪液的综合愈合。
这项研究的目的是检查由血小板衍生的生长因子(PDGF)涂层的脱细胞半月板支架在通过诱导内源性细胞迁移介导半月板撕裂的综合愈合中的潜力。将新鲜的牛半月板化学脱细胞并与肝素和PDGF-BB共价缀合。测量了体外PDGF释放动力学。将该支架移植到无血管牛半月板外植体的实验性眼泪中,并培养2周和4周。计算支架和受损外植体之间交界处的迁移和增殖细胞数以及表达PDGF受体-β(PDGFRβ)的细胞。新产生的ECM和胶原蛋白的比对通过番红O型,picrosirius红染色和微分干涉对比(DIC)进行分析。培养2周和4周后,对外植体进行拉伸测试。肝素偶联的支架显示出高水平的PDGF-BB固定化,持续释放超过2周。PDGF-BB处理的支架在无血管半月板缺损处的插入导致PDGFRβ表达增加,细胞迁移以及向缺损区的增殖。番红O-O,picrosirius红染色和DIC显示支架和受伤的外植体之间存在组织整合。用PDGF-BB涂层支架处理的外植体的拉伸特性显着高于未使用PDGF的支架。总之,PDGF-BB涂层的支架增加了PDGFRβ的表达,并促进了内源性半月板细胞向缺损区域的迁移。形成了新的基质,其桥接了天然弯液面和支架之间的空间,这与改善的生物力学性能有关。PDGF-BB涂层支架将有望用于临床修复半月板泪液。意义说明半月板撕裂是膝关节最常见的损伤。发生在内侧三分之一的最普遍的形式通常不会自发愈合,并且是膝盖骨关节炎发展的主要危险因素。该项目的目标是开发一种易于应用于临床的方法。我们选择了一种天然且容易获得的脱细胞半月板支架,并将其与PDGF偶联,我们先前发现PDGF对软骨细胞和祖细胞具有很强的趋化活性。目前的结果表明,PDGF共轭支架在无血管半月板缺陷中的插入导致内源性细胞迁移和扩散进入缺陷区,并在支架和受损外植体之间进行组织整合并改善了拉伸性能。这种PDGF共轭支架将有望用于半月板撕裂愈合的转化方法。



























 京公网安备 11010802027423号
京公网安备 11010802027423号