JAMA Surgery ( IF 16.9 ) Pub Date : 2018-07-01 , DOI: 10.1001/jamasurg.2018.0996 Georgios Antonios Margonis 1 , Stefan Buettner 1, 2 , Nikolaos Andreatos 1 , Yuhree Kim 1 , Doris Wagner 3 , Kazunari Sasaki 4 , Andrea Beer 5 , Christoph Schwarz 5 , Inger Marie Løes 6, 7 , Maria Smolle 8 , Carsten Kamphues 9 , Jin He 1 , Timothy M. Pawlik 10, 11 , Klaus Kaczirek 5 , George Poultsides 12 , Per Eystein Lønning 6, 7 , John L. Cameron 1 , Richard A. Burkhart 1 , Armin Gerger 8 , Federico N. Aucejo 4 , Martin E. Kreis 9 , Christopher L. Wolfgang 1 , Matthew J. Weiss 1
|
Importance BRAF mutations are reportedly associated with aggressive tumor biology. However, in contrast with primary colorectal cancer, the association of V600E and non-V600E BRAF mutations with survival and recurrence after resection of colorectal liver metastases (CRLM) has not been well studied.
Objective To investigate the prognostic association of BRAF mutations with survival and recurrence independently and compared with other prognostic determinants, such as KRAS mutations.
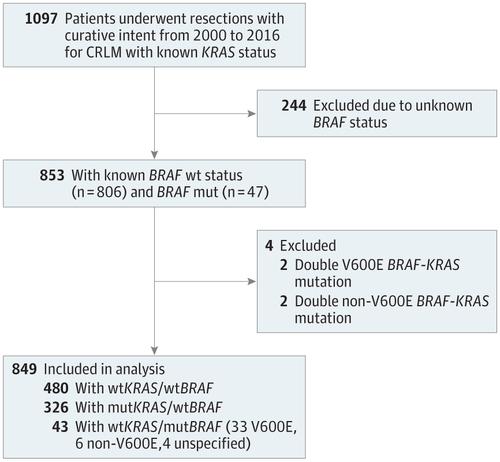
Design, Setting, and Participants In this cohort study, all patients who underwent resection for CRLM with curative intent from January 1, 2000, through December 31, 2016, at the institutions participating in the International Genetic Consortium for Colorectal Liver Metastasis and had data on BRAF and KRAS mutational status were retrospectively identified. Multivariate Cox proportional hazards regression models were used to assess long-term outcomes.
Interventions Hepatectomy in patients with CRLM.
Main Outcomes and Measures The association of V600E and non-V600E BRAF mutations with disease-free survival (DFS) and overall survival (OS).
Results Of 853 patients who met inclusion criteria (510 men [59.8%] and 343 women [40.2%]; mean [SD] age, 60.2 [12.4] years), 849 were included in the study analyses. Forty-three (5.1%) had a mutated (mut) BRAF/wild-type (wt) KRAS (V600E and non-V600E) genotype; 480 (56.5%), a wtBRAF/wtKRAS genotype; and 326 (38.4%), a wtBRAF/mutKRAS genotype. Compared with the wtBRAF/wtKRAS genotype group, patients with a mutBRAF/wtKRAS genotype more frequently were female (27 [62.8%] vs 169 [35.2%]) and 65 years or older (22 [51.2%] vs 176 [36.9%]), had right-sided primary tumors (27 [62.8%] vs 83 [17.4%]), and presented with a metachronous liver metastasis (28 [64.3%] vs 229 [46.8%]). On multivariable analysis, V600E but not non-V600E BRAF mutation was associated with worse OS (hazard ratio [HR], 2.76; 95% CI, 1.74-4.37; P < .001) and DFS (HR, 2.04; 95% CI, 1.30-3.20; P = .002). The V600E BRAF mutation had a stronger association with OS and DFS than the KRAS mutations (β for OS, 10.15 vs 2.94; β for DFS, 7.14 vs 2.27).
Conclusions and Relevance The presence of the V600E BRAF mutation was associated with worse prognosis and increased risk of recurrence. The V600E mutation was not only a stronger prognostic factor than KRAS but also was the strongest prognostic determinant in the overall cohort.
中文翻译:

手术治疗转移性结直肠肝癌患者的BRAF突变与生存和复发的关系
据报道,重要的BRAF突变与侵袭性肿瘤生物学有关。然而,与原发性结直肠癌相反,对V600E和非V600E BRAF突变与结直肠肝转移瘤(CRLM)切除后存活和复发的相关性尚未进行深入研究。
目的 探讨BRAF突变与生存和复发的预后相关性,并与其他预后决定因素(如KRAS突变)进行比较。
设计,背景和参加者 在该队列研究中,所有从2000年1月1日至2016年12月31日在国际上接受结直肠肝转移遗传学联合会研究的机构接受根治性切除术治疗的CRLM患者均获得了相关数据。回顾性鉴定了BRAF和KRAS突变状态。多变量Cox比例风险回归模型用于评估长期结果。
干预 CRLM患者的肝切除术。
主要结果和衡量指标 V600E和非V600E BRAF突变与无病生存期(DFS)和总体生存期(OS)的关联。
结果 符合纳入标准的853例患者(男性510例[59.8%]和女性343例[40.2%];平均[SD]年龄为60.2 [12.4]岁)包括849例。有43(5.1%)个具有突变(mut)的BRAF /野生型(wt)KRAS(V600E和非V600E)基因型;480(56.5%),wt BRAF / wt KRAS基因型;和326(38.4%),是野生型BRAF / mut KRAS基因型。与wt BRAF / wt KRAS基因型组相比,mut BRAF / wt KRAS患者基因型更常见的是女性(27 [62.8%]比169 [35.2%])和65岁以上(22 [51.2%]比176 [36.9%]),右侧原发肿瘤(27 [62.8%]比) 83 [17.4%]),并出现了异时肝转移(28 [64.3%]对229 [46.8%])。在多变量分析中,V600E而非非V600E的BRAF突变与较差的OS(危险比[HR],2.76; 95%CI,1.74-4.37;P <.001)和DFS(HR,2.04; 95%CI, 1.30-3.20;P = .002)。与KRAS突变相比,V600E BRAF突变与OS和DFS的关联性更强(OS的β分别为10.15与2.94; DFS的β为7.14相对于2.27)。
结论和相关性 V600E BRAF突变的存在与预后差和复发风险增加有关。V600E突变不仅是比KRAS更强的预后因素,而且还是整个队列中最强的预后决定因素。



























 京公网安备 11010802027423号
京公网安备 11010802027423号