当前位置:
X-MOL 学术
›
JAMA Intern. Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Association of the Centers for Medicare & Medicaid Services’ National Partnership to Improve Dementia Care With the Use of Antipsychotics and Other Psychotropics in Long-term Care in the United States From 2009 to 2014
JAMA Internal Medicine ( IF 39.0 ) Pub Date : 2018-05-01 , DOI: 10.1001/jamainternmed.2018.0379 Donovan T Maust 1, 2, 3 , H Myra Kim 1, 2, 3 , Claire Chiang 1, 2 , Helen C Kales 1, 2, 3, 4
JAMA Internal Medicine ( IF 39.0 ) Pub Date : 2018-05-01 , DOI: 10.1001/jamainternmed.2018.0379 Donovan T Maust 1, 2, 3 , H Myra Kim 1, 2, 3 , Claire Chiang 1, 2 , Helen C Kales 1, 2, 3, 4
Affiliation
|
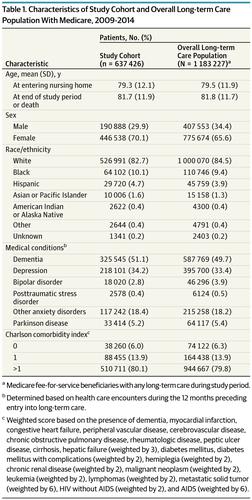
Importance The Centers for Medicare & Medicaid Services’ National Partnership to Improve Dementia Care in Nursing Homes (hereafter referred to as the partnership) was established to improve the quality of care for patients with dementia, measured by the rate of antipsychotic prescribing. Objective To determine the association of the partnership with trends in prescribing of antipsychotic and other psychotropic medication among older adults in long-term care. Design, Setting, and Participants This interrupted time-series analysis of a 20% Medicare sample from January 1, 2009, to December 31, 2014, was conducted among 637 426 fee-for-service Medicare beneficiaries in long-term care with Part D coverage. Data analysis was conducted from May 1, 2017, to January 9, 2018. Main Outcomes and Measures Quarterly prevalence of use of antipsychotic and nonantipsychotic psychotropic medications (antidepressants, mood stabilizers [eg, valproic acid and carbamazepine], benzodiazepines, and other anxiolytics or sedative-hypnotics). Results Among the 637 426 individuals in the study (446 538 women and 190 888 men; mean [SD] age at entering nursing home, 79.3 [12.1] years), psychotropic use was declining before initiation of the partnership with the exception of mood stabilizers. In the first quarter of 2009, a total of 31 056 of 145 841 patients (21.3%) were prescribed antipsychotics, which declined at a quarterly rate of –0.53% (95% CI, –0.63% to –0.44%; P < .001) until the start of the partnership. At that point, the quarterly rate of decline decreased to –0.29% (95% CI, –0.39% to –0.20%; P < .001), a postpartnership slowing of 0.24% per quarter (95% CI, 0.09%-0.39%; P = .003). The use of mood stabilizers was growing before initiation of the partnership and then accelerated after initiation of the partnership (rate, 0.22%; 95% CI, 0.18%-0.25%; P < .001; rate change, 0.14%; 95% CI, 0.10%-0.18%; P < .001), reaching 71 492 of 355 716 patients (20.1%) by the final quarter of 2014. Antidepressants were the most commonly prescribed medication overall: in the beginning of 2009, a total of 75 841 of 145 841 patients (52.0%) were prescribed antidepressants. As with antipsychotics, antidepressant use declined both before and after initiation of the partnership, but the decrease slowed (rate change, 0.34%; 95% CI, 0.18%-0.50%; P < .001). Findings were similar when limited to patients with dementia. Conclusions and Relevance Prescribing of psychotropic medications to patients in long-term care has declined, although the partnership did not accelerate this decrease. However, the use of mood stabilizers, possibly as a substitute for antipsychotics, increased and accelerated after initiation of the partnership in both long-term care residents overall and in those with dementia. Measuring use of antipsychotics alone may be an inadequate proxy for quality of care and may have contributed to a shift in prescribing to alternative medications with a poorer risk-benefit balance.
中文翻译:

2009 年至 2014 年美国医疗保险和医疗补助服务中心协会通过在长期护理中使用抗精神病药物和其他精神药物来改善痴呆症护理的全国合作伙伴关系
重要性 医疗保险和医疗补助服务中心改善疗养院痴呆症护理的全国合作伙伴关系(以下简称合作关系)的建立是为了提高痴呆症患者的护理质量,以抗精神病药处方率来衡量。目的 确定这种伙伴关系与长期护理中老年人抗精神病药和其他精神药物处方趋势的关联。设计、设置和参与者 对 2009 年 1 月 1 日至 2014 年 12 月 31 日期间 20% 医疗保险样本的中断时间序列分析,在 637 426 名接受 D 部分长期护理的按服务收费医疗保险受益人中进行覆盖。数据分析时间为2017年5月1日至2018年1月9日。主要结果和测量抗精神病药和非抗精神病药精神药物(抗抑郁药、情绪稳定剂 [例如丙戊酸和卡马西平]、苯二氮卓类药物和其他抗焦虑药或镇静催眠药)的季度使用率。结果 在研究的 637 426 名个体(446 538 名女性和 190 888 名男性;进入疗养院的平均 [SD] 年龄,79.3 [12.1] 岁)中,除情绪稳定剂外,在伙伴关系开始前,精神药物的使用正在下降. 2009 年第一季度,在 145 841 名患者中,共有 31 056 名(21.3%)服用了抗精神病药,每季度下降 –0.53%(95% CI,–0.63% 至 –0.44%;P < . 001) 直到合作关系开始。此时,季度下降率下降至 –0.29%(95% CI,–0.39% 至 –0.20%;P < .001),合作后每季度放缓 0.24%(95% CI,0.09%-0.39%;P = .003)。情绪稳定剂的使用在伙伴关系开始前增加,然后在伙伴关系开始后加速(比率,0.22%;95% CI,0.18%-0.25%;P < .001;比率变化,0.14%;95% CI , 0.10%-0.18%; P < .001),到 2014 年最后一个季度达到 355 716 名患者中的 71 492 名 (20.1%)。抗抑郁药是总体上最常用的处方药:2009 年初,共有 75 145 841 名患者中的 841 名 (52.0%) 服用了抗抑郁药。与抗精神病药一样,伙伴关系开始前后抗抑郁药的使用均有所下降,但下降速度减慢(变化率,0.34%;95% CI,0.18%-0.50%;P < .001)。当仅限于痴呆症患者时,结果是相似的。结论和相关性 为长期护理患者开出的精神药物处方有所下降,尽管合作并未加速这种下降。然而,在长期护理居民和痴呆症患者中,在建立伙伴关系后,使用情绪稳定剂(可能作为抗精神病药的替代品)增加并加速。单独衡量抗精神病药的使用可能不足以代表护理质量,并且可能导致改用风险-收益平衡较差的替代药物。在长期护理居民和痴呆症患者中,在启动伙伴关系后增加和加速。单独衡量抗精神病药的使用可能不足以代表护理质量,并且可能导致改用风险-收益平衡较差的替代药物。在长期护理居民和痴呆症患者中,在启动伙伴关系后增加和加速。单独衡量抗精神病药的使用可能不足以代表护理质量,并且可能导致改用风险收益平衡较差的替代药物。
更新日期:2018-05-01
中文翻译:

2009 年至 2014 年美国医疗保险和医疗补助服务中心协会通过在长期护理中使用抗精神病药物和其他精神药物来改善痴呆症护理的全国合作伙伴关系
重要性 医疗保险和医疗补助服务中心改善疗养院痴呆症护理的全国合作伙伴关系(以下简称合作关系)的建立是为了提高痴呆症患者的护理质量,以抗精神病药处方率来衡量。目的 确定这种伙伴关系与长期护理中老年人抗精神病药和其他精神药物处方趋势的关联。设计、设置和参与者 对 2009 年 1 月 1 日至 2014 年 12 月 31 日期间 20% 医疗保险样本的中断时间序列分析,在 637 426 名接受 D 部分长期护理的按服务收费医疗保险受益人中进行覆盖。数据分析时间为2017年5月1日至2018年1月9日。主要结果和测量抗精神病药和非抗精神病药精神药物(抗抑郁药、情绪稳定剂 [例如丙戊酸和卡马西平]、苯二氮卓类药物和其他抗焦虑药或镇静催眠药)的季度使用率。结果 在研究的 637 426 名个体(446 538 名女性和 190 888 名男性;进入疗养院的平均 [SD] 年龄,79.3 [12.1] 岁)中,除情绪稳定剂外,在伙伴关系开始前,精神药物的使用正在下降. 2009 年第一季度,在 145 841 名患者中,共有 31 056 名(21.3%)服用了抗精神病药,每季度下降 –0.53%(95% CI,–0.63% 至 –0.44%;P < . 001) 直到合作关系开始。此时,季度下降率下降至 –0.29%(95% CI,–0.39% 至 –0.20%;P < .001),合作后每季度放缓 0.24%(95% CI,0.09%-0.39%;P = .003)。情绪稳定剂的使用在伙伴关系开始前增加,然后在伙伴关系开始后加速(比率,0.22%;95% CI,0.18%-0.25%;P < .001;比率变化,0.14%;95% CI , 0.10%-0.18%; P < .001),到 2014 年最后一个季度达到 355 716 名患者中的 71 492 名 (20.1%)。抗抑郁药是总体上最常用的处方药:2009 年初,共有 75 145 841 名患者中的 841 名 (52.0%) 服用了抗抑郁药。与抗精神病药一样,伙伴关系开始前后抗抑郁药的使用均有所下降,但下降速度减慢(变化率,0.34%;95% CI,0.18%-0.50%;P < .001)。当仅限于痴呆症患者时,结果是相似的。结论和相关性 为长期护理患者开出的精神药物处方有所下降,尽管合作并未加速这种下降。然而,在长期护理居民和痴呆症患者中,在建立伙伴关系后,使用情绪稳定剂(可能作为抗精神病药的替代品)增加并加速。单独衡量抗精神病药的使用可能不足以代表护理质量,并且可能导致改用风险-收益平衡较差的替代药物。在长期护理居民和痴呆症患者中,在启动伙伴关系后增加和加速。单独衡量抗精神病药的使用可能不足以代表护理质量,并且可能导致改用风险-收益平衡较差的替代药物。在长期护理居民和痴呆症患者中,在启动伙伴关系后增加和加速。单独衡量抗精神病药的使用可能不足以代表护理质量,并且可能导致改用风险收益平衡较差的替代药物。



























 京公网安备 11010802027423号
京公网安备 11010802027423号