JAMA Psychiatry ( IF 25.8 ) Pub Date : 2018-04-01 , DOI: 10.1001/jamapsychiatry.2017.4585 Margarita Alegria 1, 2, 3 , Ora Nakash 1, 4 , Kirsten Johnson 5 , Andrea Ault-Brutus 6 , Nicholas Carson 3, 7 , Mirko Fillbrunn 1, 2 , Ye Wang 1 , Alice Cheng 8 , Treniece Harris 3, 9 , Antonio Polo 10 , Alisa Lincoln 11 , Elmer Freeman 12, 13 , Benjamin Bostdorf 14 , Marcos Rosenbaum 15 , Claudia Epelbaum 16 , Martin LaRoche 3, 17 , Ebele Okpokwasili-Johnson 18 , MaJose Carrasco 19 , Patrick E. Shrout 20
|
Importance Few randomized clinical trials have been conducted with ethnic/racial minorities to improve shared decision making (SDM) and quality of care.
Objective To test the effectiveness of patient and clinician interventions to improve SDM and quality of care among an ethnically/racially diverse sample.
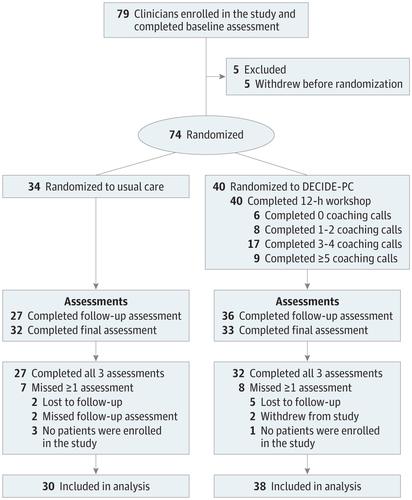
Design, Setting, and Participants This cross-level 2 × 2 randomized clinical trial included clinicians at level 2 and patients (nested within clinicians) at level 1 from 13 Massachusetts behavioral health clinics. Clinicians and patients were randomly selected at each site in a 1:1 ratio for each 2-person block. Clinicians were recruited starting September 1, 2013; patients, starting November 3, 2013. Final data were collected on September 30, 2016. Data were analyzed based on intention to treat.
Interventions The clinician intervention consisted of a workshop and as many as 6 coaching telephone calls to promote communication and therapeutic alliance to improve SDM. The 3-session patient intervention sought to improve SDM and quality of care.
Main Outcomes and Measures The SDM was assessed by a blinded coder based on clinical recordings, patient perception of SDM and quality of care, and clinician perception of SDM.
Results Of 312 randomized patients, 212 (67.9%) were female and 100 (32.1%) were male; mean (SD) age was 44.0 (15.0) years. Of 74 randomized clinicians, 56 (75.7%) were female and 18 (4.3%) were male; mean (SD) age was 39.8 (12.5) years. Patient-clinician pairs were assigned to 1 of the following 4 design arms: patient and clinician in the control condition (n = 72), patient in intervention and clinician in the control condition (n = 68), patient in the control condition and clinician in intervention (n = 83), or patient and clinician in intervention (n = 89). All pairs underwent analysis. The clinician intervention significantly increased SDM as rated by blinded coders using the 12-item Observing Patient Involvement in Shared Decision Making instrument (b = 4.52; SE = 2.17; P = .04; Cohen d = 0.29) but not as assessed by clinician or patient. More clinician coaching sessions (dosage) were significantly associated with increased SDM as rated by blinded coders (b = 12.01; SE = 3.72; P = .001; Cohen d = 0.78). The patient intervention significantly increased patient-perceived quality of care (b = 2.27; SE = 1.16; P = .05; Cohen d = 0.19). There was a significant interaction between patient and clinician dosage (b = 7.40; SE = 3.56; P = .04; Cohen d = 0.62), with the greatest benefit when both obtained the recommended dosage.
Conclusions and Relevance The clinician intervention could improve SDM with minority populations, and the patient intervention could augment patient-reported quality of care.
Trial Registration clinicaltrials.gov Identifier: NCT01947283
中文翻译:

DECIDE干预在多文化患者行为健康中的共同决策和可感知的护理质量方面的有效性随机临床试验
重要性 很少有针对少数族裔/种族的随机临床试验来改善共同决策(SDM)和护理质量。
目的 测试在种族/种族差异样本中,患者和临床医生干预措施改善SDM和护理质量的有效性。
设计,设置和参与者 这项跨水平的2×2随机临床试验包括来自马萨诸塞州13家行为健康诊所的2级临床医生和1级的患者(嵌套在临床医生内)。对于每个2人病区,以1:1的比例在每个位置随机选择临床医生和患者。从2013年9月1日开始招募临床医生;患者于2013年11月3日开始。最终数据于2016年9月30日收集。根据治疗意向对数据进行了分析。
干预 临床医生的干预包括一个讲习班和多达6个教练电话,以促进沟通和治疗联盟以改善SDM。为期3天的患者干预旨在改善SDM和护理质量。
主要结果和措施 SDM由盲人编码者根据临床记录,患者对SDM的认知和护理质量以及临床医生对SDM的认知进行评估。
结果 312例随机分组的患者中,女性212例(67.9%),男性100例(32.1%)。平均(SD)年龄为44.0(15.0)岁。在74名随机临床医生中,女性56名(75.7%),男性18名(4.3%)。平均(SD)年龄为39.8(12.5)岁。将患者-临床医生对分配给以下4个设计组中的1个:处于控制状态的患者和临床医生(n = 72),处于介入状态的患者和处于控制状态的临床医生(n = 68),处于控制条件下的患者和临床医生干预(n = 83),或患者和临床医生进行干预(n = 89)。所有对都进行了分析。盲人编码者使用12项观察患者参与共享决策制定工具的干预措施,临床医生的干预显着提高了SDM(b = 4.52; SE = 2.17;P = .04; Cohen d = 0.29),但未经临床医生或患者评估。如盲人编码者所评定的那样,更多的临床医师指导课程(剂量)与SDM的增加显着相关(b = 12.01; SE = 3.72;P = .001; Cohen d = 0.78)。患者干预显着提高了患者感知的护理质量(b = 2.27; SE = 1.16;P = 0.05; Cohen d = 0.19)。患者和临床医生的剂量之间存在显着的相互作用(b = 7.40; SE = 3.56;P = .04; Cohen d = 0.62),当两者都获得推荐剂量时,获益最大。
结论和相关性 临床医生的干预可以改善少数人群的SDM,患者的干预可以提高患者报告的护理质量。
试验注册 临床试验.gov标识符:NCT01947283


























 京公网安备 11010802027423号
京公网安备 11010802027423号