JAMA Oncology ( IF 28.4 ) Pub Date : 2018-04-01 , DOI: 10.1001/jamaoncol.2017.4942 Kara A Michels 1 , Ruth M Pfeiffer 1 , Louise A Brinton 1 , Britton Trabert 1
|
Importance Although oral contraceptive (OC) use is common, the influence of OC use on carcinogenesis is not fully understood. A recent Agency for Healthcare Research and Quality report identified a need to understand the consistency of OC use and cancer associations across subpopulations, including smokers and obese women.
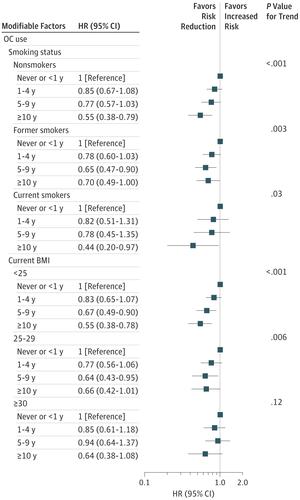
Objective To determine whether associations between duration of OC use and risk of specific cancers were modified by lifestyle characteristics.
Design, Setting, and Participants The prospective NIH-AARP Diet and Health Study (enrolled 1995-1996, followed until 2011), with population-based recruitment of AARP members in 6 states and 2 metropolitan areas. All analyses included at least 100 000 women who reported OC use at enrollment. We identified 1241 ovarian, 2337 endometrial, 11 114 breast, and 3507 colorectal cancer cases during follow-up. Data analysis was performed between September 2016 and April 2017.
Exposures Duration of OC use (never or <1 year [reference], 1-4, 5-9, or ≥10 years).
Main Outcomes and Measures Development of ovarian, endometrial, breast, and colorectal cancers. We examined effect modification by modifiable lifestyle characteristics: cigarette smoking, alcohol consumption, body mass index (BMI), and physical activity. We used Cox models adjusted for age, race, age at menarche, and the modifiers of interest.
Results The analytic population was aged 50 to 71 years (median, 62 years) at enrollment and largely white (91%) and postmenopausal (96%). For ovarian cancer, OC use–associated risk reductions strengthened with duration of use (long-term OC use [≥10 years] HR, 0.60; 95% CI, 0.47-0.76; P < .001 for trend) and were similar across modifiable lifestyle factors. Risk reductions for endometrial cancer strengthened with duration of use (long-term OC use HR, 0.66; 95% CI, 0.56-0.78; P < .001 for trend); the most pronounced reductions were among long-term OC users who were smokers (HR, 0.47; 95% CI, 0.25-0.88), had obese BMIs (0.36; 95% CI, 0.25-0.52), and who exercised rarely (HR, 0.40; 95% CI, 0.29-0.56). Associations between OC use and breast and colorectal cancers were predominantly null.
Conclusions and Relevance Long-term OC use is consistently associated with reduced ovarian cancer risk across lifestyle factors. We observed the greatest risk reductions for endometrial cancer among women at risk for chronic diseases (ie, smokers, obese BMI). Oral contraceptive use may be beneficial for chemoprevention for a range of women with differing baseline cancer risks.
中文翻译:

修改口服避孕药使用时间与卵巢癌、子宫内膜癌、乳腺癌和结直肠癌之间的关系
重要性 虽然口服避孕药 (OC) 的使用很常见,但 OC 使用对致癌作用的影响尚不完全清楚。医疗保健研究和质量机构最近的一份报告指出,需要了解 OC 使用的一致性和跨亚群(包括吸烟者和肥胖女性)的癌症关联。
目的 确定 OC 使用时间与特定癌症风险之间的关联是否会因生活方式特征而改变。
设计、设置和参与者 前瞻性 NIH-AARP 饮食与健康研究(1995-1996 年入组,一直到 2011 年),在 6 个州和 2 个大都市地区以人口为基础招募 AARP 成员。所有分析都包括至少 100 000 名在登记时报告使用 OC 的女性。我们在随访期间确定了 1241 例卵巢癌、2337 例子宫内膜癌、11114 例乳腺癌和 3507 例结直肠癌病例。数据分析于 2016 年 9 月至 2017 年 4 月期间进行。
暴露 OC 使用的持续时间(从不或 <1 年 [参考]、1-4、5-9 或 ≥10 年)。
主要结果和措施 卵巢癌、子宫内膜癌、乳腺癌和结直肠癌的发展。我们通过可改变的生活方式特征检查了效果修改:吸烟、饮酒、体重指数 (BMI) 和身体活动。我们使用根据年龄、种族、初潮年龄和感兴趣的修正因素调整的 Cox 模型。
结果 分析人群在入组时年龄为 50 至 71 岁(中位数为 62 岁),大部分为白人(91%)和绝经后(96%)。对于卵巢癌,OC 使用相关的风险降低随着使用时间的延长而增强(长期 OC 使用 [≥10 年] HR,0.60;95% CI,0.47-0.76;趋势P < .001)并且在可修改的范围内相似生活方式因素。随着使用时间的延长,子宫内膜癌的风险降低得到加强(长期 OC 使用 HR,0.66;95% CI,0.56-0.78;P < .001 表示趋势);最显着的减少发生在吸烟者(HR,0.47;95% CI,0.25-0.88)、肥胖 BMI(0.36;95% CI,0.25-0.52)和很少锻炼(HR, 0.40;95% CI,0.29-0.56)。OC 使用与乳腺癌和结直肠癌之间的关联主要是无效的。
结论和相关性 长期使用 OC 始终与降低各种生活方式因素的卵巢癌风险相关。我们观察到有慢性病风险的女性(即吸烟者、肥胖 BMI)的子宫内膜癌风险降低幅度最大。对于具有不同基线癌症风险的一系列女性,口服避孕药的使用可能有益于化学预防。


























 京公网安备 11010802027423号
京公网安备 11010802027423号