JAMA Surgery ( IF 16.9 ) Pub Date : 2018-05-01 , DOI: 10.1001/jamasurg.2017.5449 Morgan M. Sellers 1 , Luke J. Keele 2 , Catherine E. Sharoky 1 , Christopher Wirtalla 1 , Elizabeth A. Bailey 1 , Rachel R. Kelz 1
|
Importance Important metrics of residency program success include the clinical outcomes achieved by trainees after transitioning to practice. Previous studies have shown significant differences in reported training experiences of general surgery residents at nonuniversity-based residency (NUBR) and university-based residency (UBR) programs.
Objective To examine the differences in practice patterns and clinical outcomes between surgeons trained in NUBR and those trained in UBR programs.
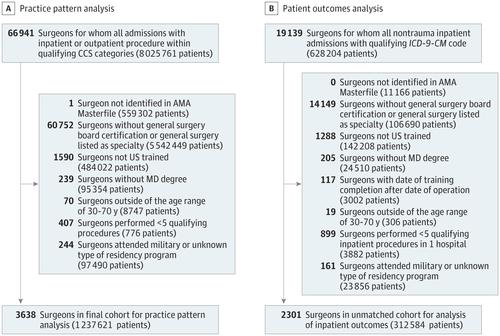
Design, Setting, and Participants This observational cohort study linked the claims data of patients who underwent general surgery procedures in New York, Florida, and Pennsylvania between January 1, 2012, and December 31, 2013, to demographic and training information of surgeons in the American Medical Association Physician Masterfile. Patients who underwent a qualifying procedure were grouped by surgeon. Practice pattern analysis was performed on 3638 surgeons and 1 237 621 patients, representing 214 residency programs. Clinical outcomes analysis was performed on 2301 surgeons and 312 584 patients. Data analysis was conducted from February 1, 2017, to July 31, 2017.
Exposures NUBR or UBR training status.
Main Outcomes and Measures Inpatient mortality, complications, and prolonged length of stay.
Results No significant differences were observed between the NUBR-trained surgeons and UBR-trained surgeons in age (mean, 53.3 years vs 53.7 years), sex (female, 18.2% vs 16.9%), or years of clinical experience (mean, 16.5 years vs 16.5 years). Overall, NUBR-trained surgeons compared with UBR-trained surgeons performed more procedures (median interquartile range [IQR], 328 [93-661] vs 164 [49-444]; P < .001) and performed a greater proportion of procedures in the outpatient setting (risk difference, 6.5; 95% CI, 6.4 to 6.7; P < .001). Before matching, the mean proportion of patients with documented inpatient mortality was lower for NUBR-trained surgeons than for UBR-trained surgeons (risk difference, −1.01; 95% CI, −1.41 to −0.61; P < .001). The mean proportion of patients with complications (risk difference, −3.17%; 95% CI, −4.21 to −2.13; P < .001) and prolonged length of stay (risk difference, −1.89%; 95% CI, −2.79 to −0.98; P < .001) was also lower for NUBR-trained surgeons. After matching, no significant differences in patient mortality, complications, and prolonged length of stay were found between NUBR- and UBR-trained surgeons.
Conclusions and Relevance Surgeons trained in NUBR and UBR programs have distinct practice patterns. After controlling for patient, procedure, and hospital factors, no differences were observed in the inpatient outcomes between the 2 groups.
中文翻译:

在大学或非大学的住院医师培训计划中,手术实践模式和临床结果与外科医生培训的关联
重要性 居留计划成功的重要指标包括学员在过渡到实践后所取得的临床成果。先前的研究表明,在非大学为基础的居留(NUBR)和大学为基础的居留(UBR)计划下,普通外科手术住院医师的培训经历报告存在显着差异。
目的 探讨在NUBR中接受培训的外科医生与在UBR计划中接受培训的外科医生在实践模式和临床结果方面的差异。
设计,地点和参与者 这项观察性队列研究将2012年1月1日至2013年12月31日期间在纽约,佛罗里达和宾夕法尼亚州进行了普外科手术的患者的索赔数据与该州外科医生的人口统计信息和培训信息相关联。美国医学会医师主文件。接受资格检查的患者按外科医生分组。对3638名外科医生和1 237 621名患者进行了实践模式分析,代表214个住院医师计划。对2301名外科医生和312 584名患者进行了临床结局分析。数据分析于2017年2月1日至2017年7月31日进行。
暴露 NUBR或UBR训练状态。
主要结果和衡量指标 住院病人的死亡率,并发症和延长的住院时间。
结果 接受NUBR培训的外科医生与受UBBR培训的外科医生在年龄(平均53.3岁vs 53.7岁),性别(女性,18.2%vs 16.9%)或多年临床经验(平均16.5岁)之间没有显着差异。与16.5年相比)。总体而言,与UBBR训练的外科医生相比,NUBR训练的外科医生执行了更多的手术(中四分位间距[IQR],328 [93-661]与164 [49-444];P <.001),并且在门诊环境(风险差异6.5; 95%CI为6.4至6.7; P <0.001)。在匹配之前,接受NUBR培训的外科医生的住院死亡率已记录的平均比例要低于接受UBR培训的外科医生的平均比例(风险差异为-1.01; 95%CI为-1.41至-0.61;P <.001)。合并症患者的平均比例(风险差异-3.17%; 95%CI,-4.21至-2.13; P <.001)和延长的住院时间(风险差异-1.89%; 95%CI,-2.79至- −0.98;P <.001)对于接受NUBR培训的外科医生也较低。匹配后,在接受NUBR和UBR培训的外科医生之间,在患者死亡率,并发症和住院时间延长方面无显着差异。
结论和相关性 在NUBR和UBR计划中接受培训的外科医生具有不同的练习模式。在控制了患者,手术和医院因素之后,两组之间的住院结局没有差异。


























 京公网安备 11010802027423号
京公网安备 11010802027423号