当前位置:
X-MOL 学术
›
J. Am. Coll. Cardiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Relationship of Aging and Incident Comorbidities to Stroke Risk in Patients With Atrial Fibrillation
Journal of the American College of Cardiology ( IF 24.0 ) Pub Date : 2018-01-01 , DOI: 10.1016/j.jacc.2017.10.085 Tze-Fan Chao , Gregory Y.H. Lip , Chia-Jen Liu , Yenn-Jiang Lin , Shih-Lin Chang , Li-Wei Lo , Yu-Feng Hu , Ta-Chuan Tuan , Jo-Nan Liao , Fa-Po Chung , Tzeng-Ji Chen , Shih-Ann Chen
Journal of the American College of Cardiology ( IF 24.0 ) Pub Date : 2018-01-01 , DOI: 10.1016/j.jacc.2017.10.085 Tze-Fan Chao , Gregory Y.H. Lip , Chia-Jen Liu , Yenn-Jiang Lin , Shih-Lin Chang , Li-Wei Lo , Yu-Feng Hu , Ta-Chuan Tuan , Jo-Nan Liao , Fa-Po Chung , Tzeng-Ji Chen , Shih-Ann Chen
|
BACKGROUND
When assessing ischemic stroke risk in patients with atrial fibrillation (AF), the CHA2DS2-VASc score is calculated based on the baseline risk factors, and the outcomes are determined after a follow-up period. However, the stroke risk in patients with AF does not remain static, and with time, patients get older and accumulate more comorbidities. OBJECTIVES
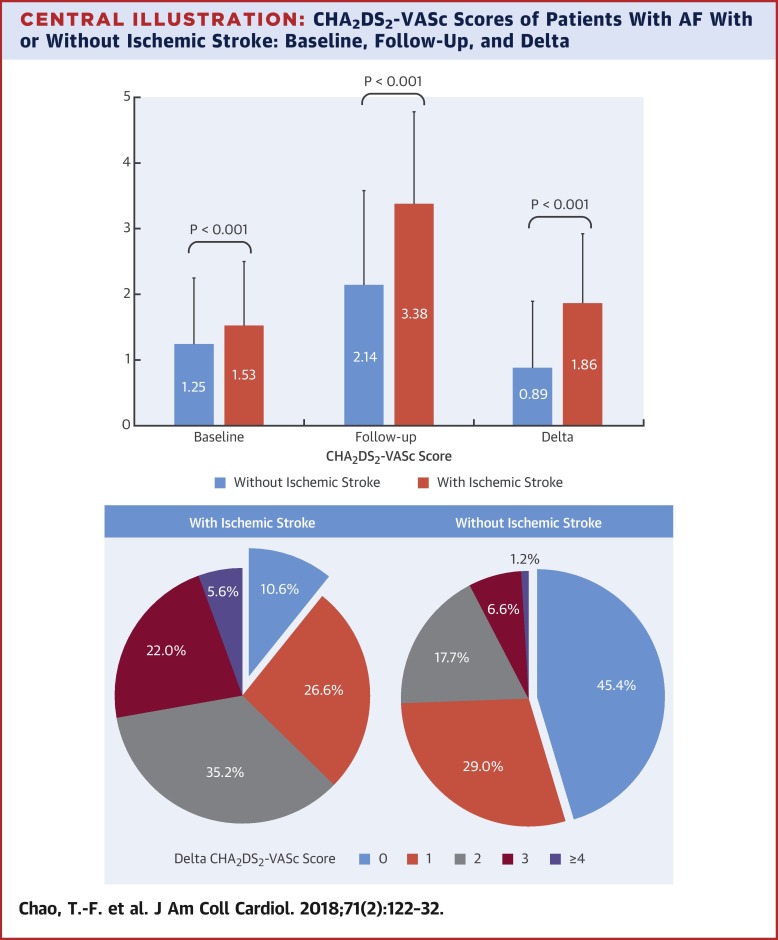
This study hypothesized that the "Delta CHA2DS2-VASc score," which reflects the change in score between baseline and follow-up, would be more predictive of ischemic stroke compared with the baseline CHA2DS2-VASc score. METHODS
A total of 31,039 patients with AF who did not receive antiplatelet agents or oral anticoagulants, and who did not have comorbidities of the CHA2DS2-VASc score except for age and sex, were studied. The Delta CHA2DS2-VASc scores were defined as the differences between the baseline and follow-up CHA2DS2-VASc scores. During 171,956 person-years, 4,103 patients experienced ischemic stroke. The accuracies of baseline, follow-up, and Delta CHA2DS2-VASc scores in predicting ischemic stroke were analyzed and compared. RESULTS
The mean baseline CHA2DS2-VASc score was 1.29, which increased to 2.31 during the follow-up, with a mean Delta CHA2DS2-VASc score of 1.02. The CHA2DS2-VASc score remained unchanged in only 40.8% of patients. Among 4,103 patients who experienced ischemic stroke, 89.4% had a Delta CHA2DS2-VASc score ≥1 compared with only 54.6% in patients without ischemic stroke, and 2,643 (64.4%) patients had ≥1 new-onset comorbidity, the most common being hypertension. The Delta CHA2DS2-VASc score was a significant predictor of ischemic stroke that performed better than baseline or follow-up CHA2DS2-VASc scores, as assessed by the C-index and the net reclassification index. CONCLUSIONS
In this AF cohort, the authors demonstrated that the CHA2DS2-VASc score was not static, and that most patients with AF developed ≥1 new stroke risk factor before presentation with ischemic stroke. The Delta CHA2DS2-VASc score, reflecting the change in score between baseline and follow-up, was strongly predictive of ischemic stroke, reflecting how stroke risk in AF is a dynamic process due to increasing age and incident comorbidities.
中文翻译:

心房颤动患者衰老和合并症与卒中风险的关系
背景 在评估房颤(AF)患者缺血性卒中风险时,CHA2DS2-VASc 评分是根据基线风险因素计算的,并在随访期后确定结果。然而,房颤患者的卒中风险并不是一成不变的,随着时间的推移,患者会变老并积累更多的合并症。目的 本研究假设,与基线 CHA2DS2-VASc 评分相比,反映基线和随访之间评分变化的“Delta CHA2DS2-VASc 评分”将更能预测缺血性卒中。方法共研究了 31,039 名未接受抗血小板药物或口服抗凝剂治疗且除年龄和性别外没有 CHA2DS2-VASc 评分合并症的 AF 患者。Delta CHA2DS2-VASc 评分定义为基线和随访 CHA2DS2-VASc 评分之间的差异。在 171,956 人年期间,4,103 名患者经历了缺血性中风。分析和比较了基线、随访和 Delta CHA2DS2-VASc 评分预测缺血性卒中的准确性。结果 平均基线 CHA2DS2-VASc 评分为 1.29,在随访期间增加至 2.31,平均 Delta CHA2DS2-VASc 评分为 1.02。只有 40.8% 的患者 CHA2DS2-VASc 评分保持不变。在经历过缺血性卒中的 4,103 名患者中,89.4% 的 Delta CHA2DS2-VASc 评分≥1,而在没有缺血性卒中的患者中只有 54.6%,并且 2,643 (64.4%) 名患者有≥1 种新发合并症,最常见的是高血压. Delta CHA2DS2-VASc 评分是缺血性卒中的重要预测指标,其表现优于基线或随访 CHA2DS2-VASc 评分,由 C 指数和净重分类指数评估。结论 在这个 AF 队列中,作者证明 CHA2DS2-VASc 评分不是静态的,并且大多数 AF 患者在出现缺血性卒中之前就出现了≥1 个新的卒中危险因素。Delta CHA2DS2-VASc 评分反映了基线和随访之间的评分变化,强烈预测缺血性卒中,反映了 AF 的卒中风险是如何随着年龄的增加和并发症的增加而成为一个动态过程。作者证明 CHA2DS2-VASc 评分不是一成不变的,并且大多数 AF 患者在出现缺血性卒中之前就出现了≥1 个新的卒中危险因素。Delta CHA2DS2-VASc 评分反映了基线和随访之间的评分变化,强烈预测缺血性卒中,反映了 AF 的卒中风险是如何随着年龄的增加和并发症的增加而成为一个动态过程。作者证明 CHA2DS2-VASc 评分不是一成不变的,并且大多数 AF 患者在出现缺血性卒中之前就出现了≥1 个新的卒中危险因素。Delta CHA2DS2-VASc 评分反映了基线和随访之间的评分变化,强烈预测缺血性卒中,反映了 AF 的卒中风险是如何随着年龄的增加和并发症的增加而成为一个动态过程。
更新日期:2018-01-01
中文翻译:

心房颤动患者衰老和合并症与卒中风险的关系
背景 在评估房颤(AF)患者缺血性卒中风险时,CHA2DS2-VASc 评分是根据基线风险因素计算的,并在随访期后确定结果。然而,房颤患者的卒中风险并不是一成不变的,随着时间的推移,患者会变老并积累更多的合并症。目的 本研究假设,与基线 CHA2DS2-VASc 评分相比,反映基线和随访之间评分变化的“Delta CHA2DS2-VASc 评分”将更能预测缺血性卒中。方法共研究了 31,039 名未接受抗血小板药物或口服抗凝剂治疗且除年龄和性别外没有 CHA2DS2-VASc 评分合并症的 AF 患者。Delta CHA2DS2-VASc 评分定义为基线和随访 CHA2DS2-VASc 评分之间的差异。在 171,956 人年期间,4,103 名患者经历了缺血性中风。分析和比较了基线、随访和 Delta CHA2DS2-VASc 评分预测缺血性卒中的准确性。结果 平均基线 CHA2DS2-VASc 评分为 1.29,在随访期间增加至 2.31,平均 Delta CHA2DS2-VASc 评分为 1.02。只有 40.8% 的患者 CHA2DS2-VASc 评分保持不变。在经历过缺血性卒中的 4,103 名患者中,89.4% 的 Delta CHA2DS2-VASc 评分≥1,而在没有缺血性卒中的患者中只有 54.6%,并且 2,643 (64.4%) 名患者有≥1 种新发合并症,最常见的是高血压. Delta CHA2DS2-VASc 评分是缺血性卒中的重要预测指标,其表现优于基线或随访 CHA2DS2-VASc 评分,由 C 指数和净重分类指数评估。结论 在这个 AF 队列中,作者证明 CHA2DS2-VASc 评分不是静态的,并且大多数 AF 患者在出现缺血性卒中之前就出现了≥1 个新的卒中危险因素。Delta CHA2DS2-VASc 评分反映了基线和随访之间的评分变化,强烈预测缺血性卒中,反映了 AF 的卒中风险是如何随着年龄的增加和并发症的增加而成为一个动态过程。作者证明 CHA2DS2-VASc 评分不是一成不变的,并且大多数 AF 患者在出现缺血性卒中之前就出现了≥1 个新的卒中危险因素。Delta CHA2DS2-VASc 评分反映了基线和随访之间的评分变化,强烈预测缺血性卒中,反映了 AF 的卒中风险是如何随着年龄的增加和并发症的增加而成为一个动态过程。作者证明 CHA2DS2-VASc 评分不是一成不变的,并且大多数 AF 患者在出现缺血性卒中之前就出现了≥1 个新的卒中危险因素。Delta CHA2DS2-VASc 评分反映了基线和随访之间的评分变化,强烈预测缺血性卒中,反映了 AF 的卒中风险是如何随着年龄的增加和并发症的增加而成为一个动态过程。



























 京公网安备 11010802027423号
京公网安备 11010802027423号