PLOS Medicine ( IF 15.8 ) Pub Date : 2017-12-27 , DOI: 10.1371/journal.pmed.1002475 Christine Johnston , Amalia Magaret , Pavitra Roychoudhury , Alexander L. Greninger , Daniel Reeves , Joshua Schiffer , Keith R. Jerome , Cassandra Sather , Kurt Diem , Jairam R. Lingappa , Connie Celum , David M. Koelle , Anna Wald
|
Background
Quantitative estimation of the extent to which the immune system’s protective effect against one herpes simplex virus type 2 (HSV-2) infection protects against infection with additional HSV-2 strains is important for understanding the potential for HSV-2 vaccine development. Using viral genotyping, we estimated the prevalence of HSV-2 dual-strain infection and identified risk factors.
Methods and findings
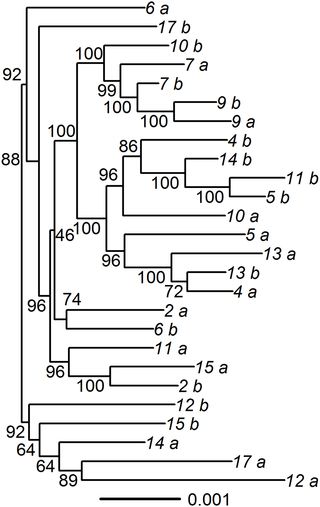
People with and without HIV infection participating in HSV-2 natural history studies (University of Washington Virology Research Clinic) and HIV prevention trials (HIV Prevention Trials Network 039 and Partners in Prevention HSV/HIV Transmission Study) in the US, Africa, and Peru with 2 genital specimens each containing ≥105 copies herpes simplex virus DNA/ml collected a median of 5 months apart (IQR: 2–11 months) were included. It is unlikely that 2 strains would be detected in the same sample simultaneously; therefore, 2 samples were required to detect dual-strain infection. We identified 85 HSV-2 SNPs that, in aggregate, could determine whether paired HSV-2 strains were the same or different with >90% probability. These SNPs were then used to create a customized high-throughput array-based genotyping assay. Participants were considered to be infected with more than 1 strain of HSV-2 if their samples differed by ≥5 SNPs between the paired samples, and dual-strain infection was confirmed using high-throughput sequencing (HTS). We genotyped pairs of genital specimens from 459 people; 213 (46%) were men, the median age was 34 years (IQR: 27–44), and 130 (28%) were HIV seropositive. Overall, 272 (59%) people were from the US, 59 (13%) were from Peru, and 128 (28%) were from 8 countries in Africa. Of the 459 people, 18 (3.9%) met the criteria for dual-strain infection. HTS and phylogenetic analysis of paired specimens confirmed shedding of 2 distinct HSV-2 strains collected at different times in 17 pairs, giving an estimated dual-strain infection prevalence of 3.7% (95% CI = 2.0%–5.4%). Paired samples with dual-strain infection differed by a median of 274 SNPs in the UL_US region (range 129–413). Matching our observed dual-strain infection frequency to simulated data of varying prevalences and allowing only 2 samples per person, we inferred the true prevalence of dual-strain infection to be 7%. In multivariable analysis, controlling for HIV status and continent of origin, people from Africa had a higher risk for dual-strain infection (risk ratio [RR] = 9.20, 95% CI = 2.05–41.32), as did people who were HIV seropositive (RR = 4.06, 95% CI = 1.42–11.56).
Conclusions
HSV-2 dual-strain infection was detected in 3.7% of paired samples from individual participants, and was more frequent among people with HIV infection. Simulations suggest that the true prevalence of dual-strain infection is 7%. Our data indicate that naturally occurring immunity to HSV-2 may be protective against infection with a second strain. This study is limited by the inability to determine the timing of acquisition of the second strain.
中文翻译:

美国,秘鲁和撒哈拉以南非洲的8个国家的双株2型生殖器单纯疱疹病毒2型(HSV-2)感染:巢式截面病毒基因分型研究
背景
定量估计免疫系统对一种2型单纯疱疹病毒(HSV-2)感染的保护作用可防止其他HSV-2株感染的程度,对于理解HSV-2疫苗开发的潜力很重要。使用病毒基因分型,我们估计了HSV-2双株感染的患病率,并确定了危险因素。
方法和发现
患有或未感染HIV的人参加了美国,非洲和秘鲁的HSV-2自然史研究(华盛顿大学病毒学研究诊所)和HIV预防试验(HIV预防试验网络039和预防HSV / HIV传播合作伙伴)。 2个生殖器标本,每个样本均≥10 5包括平均间隔5个月(IQR:2-11个月)收集的单纯疱疹病毒DNA / ml拷贝数。在同一样品中不可能同时检测到2个菌株。因此,需要2个样本来检测双株感染。我们确定了85个HSV-2 SNP,这些SNP合计可以确定配对的HSV-2菌株是相同还是不同,可能性> 90%。然后将这些SNP用于创建定制的基于高通量阵列的基因分型分析。如果参与者的样品在配对样品之间的差异大于或等于5个SNP,则认为参与者感染了1株以上的HSV-2,并且使用高通量测序(HTS)确认了双株感染。我们对459人的生殖器标本进行了基因分型。213名(46%)是男性,中位年龄为34岁(IQR:27-44),130例(28%)为HIV血清反应阳性。总体而言,有272人(59%)来自美国,有59人(13%)来自秘鲁,有128人(28%)来自非洲的8个国家。在459人中,有18人(3.9%)达到了双株感染的标准。HTS和配对标本的系统发育分析证实,在17个对中,在不同时间收集了2个不同的HSV-2株脱落,估计双株感染率为3.7%(95%CI = 2.0%–5.4%)。带有双毒株感染的配对样本在U中的中位数为274个SNP HTS和配对标本的系统发育分析证实,在17个对中,在不同时间收集了2个不同的HSV-2株脱落,估计双株感染率为3.7%(95%CI = 2.0%–5.4%)。带有双毒株感染的配对样本在U中的中位数为274个SNP HTS和配对标本的系统发育分析证实,在17个对中,在不同时间收集了2个不同的HSV-2株脱落,估计双株感染率为3.7%(95%CI = 2.0%–5.4%)。带有双毒株感染的配对样本在U中的中位数为274个SNPL _U S区域(范围129–413)。将我们观察到的双株感染频率与不同患病率的模拟数据进行匹配,并且每人仅允许2个样本,我们推断双株感染的真实患病率为7%。在多变量分析中,控制艾滋病毒状况和原产国,非洲人与双株感染的风险较高(风险比[RR] = 9.20,95%CI = 2.05–41.32),HIV阳性的人也是如此。 (RR = 4.06,95%CI = 1.42-11.56)。
结论
在个人参与者的配对样本中,有3.7%的人检测到HSV-2双株感染,并且在HIV感染者中更为常见。模拟表明,双株感染的真实患病率为7%。我们的数据表明,天然存在的对HSV-2的免疫力可能对第二种菌株的感染具有保护作用。这项研究受到无法确定第二个菌株获取时间的限制。


























 京公网安备 11010802027423号
京公网安备 11010802027423号