Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Association of Broad- vs Narrow-Spectrum Antibiotics With Treatment Failure, Adverse Events, and Quality of Life in Children With Acute Respiratory Tract Infections
JAMA ( IF 120.7 ) Pub Date : 2017-12-19 , DOI: 10.1001/jama.2017.18715 Jeffrey S Gerber 1, 2, 3 , Rachael K Ross 1 , Matthew Bryan 3 , A Russell Localio 3 , Julia E Szymczak 3 , Richard Wasserman 4 , Darlene Barkman 5 , Folasade Odeniyi 1 , Kathryn Conaboy 5 , Louis Bell 1, 6 , Theoklis E Zaoutis 1, 2, 3 , Alexander G Fiks 1, 3, 6
JAMA ( IF 120.7 ) Pub Date : 2017-12-19 , DOI: 10.1001/jama.2017.18715 Jeffrey S Gerber 1, 2, 3 , Rachael K Ross 1 , Matthew Bryan 3 , A Russell Localio 3 , Julia E Szymczak 3 , Richard Wasserman 4 , Darlene Barkman 5 , Folasade Odeniyi 1 , Kathryn Conaboy 5 , Louis Bell 1, 6 , Theoklis E Zaoutis 1, 2, 3 , Alexander G Fiks 1, 3, 6
Affiliation
|
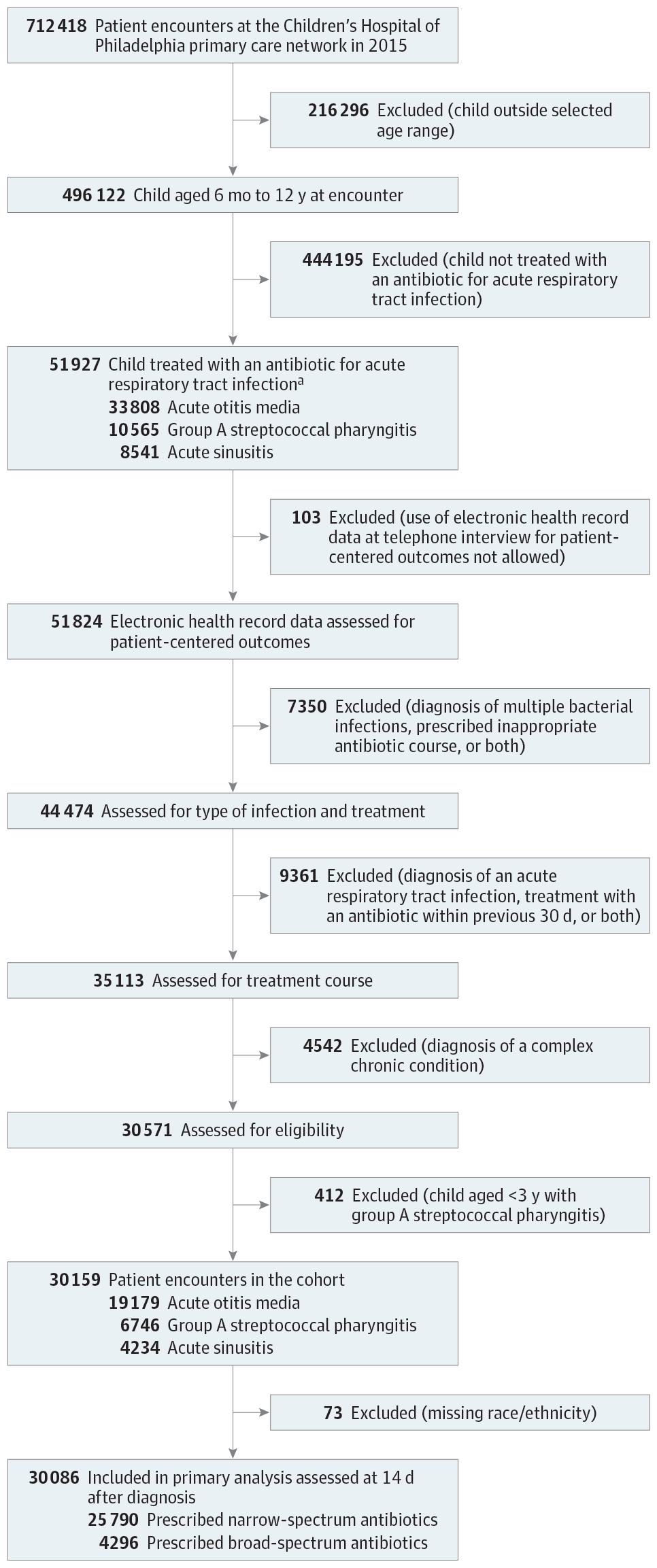
Importance Acute respiratory tract infections account for the majority of antibiotic exposure in children, and broad-spectrum antibiotic prescribing for acute respiratory tract infections is increasing. It is not clear whether broad-spectrum treatment is associated with improved outcomes compared with narrow-spectrum treatment. Objective To compare the effectiveness of broad-spectrum and narrow-spectrum antibiotic treatment for acute respiratory tract infections in children. Design, Setting, and Participants A retrospective cohort study assessing clinical outcomes and a prospective cohort study assessing patient-centered outcomes of children between the ages of 6 months and 12 years diagnosed with an acute respiratory tract infection and prescribed an oral antibiotic between January 2015 and April 2016 in a network of 31 pediatric primary care practices in Pennsylvania and New Jersey. Stratified and propensity score–matched analyses to account for confounding by clinician and by patient-level characteristics, respectively, were implemented for both cohorts. Exposures Broad-spectrum antibiotics vs narrow-spectrum antibiotics. Main Outcomes and Measures In the retrospective cohort, the primary outcomes were treatment failure and adverse events 14 days after diagnosis. In the prospective cohort, the primary outcomes were quality of life, other patient-centered outcomes, and patient-reported adverse events. Results Of 30 159 children in the retrospective cohort (19 179 with acute otitis media; 6746, group A streptococcal pharyngitis; and 4234, acute sinusitis), 4307 (14%) were prescribed broad-spectrum antibiotics including amoxicillin-clavulanate, cephalosporins, and macrolides. Broad-spectrum treatment was not associated with a lower rate of treatment failure (3.4% for broad-spectrum antibiotics vs 3.1% for narrow-spectrum antibiotics; risk difference for full matched analysis, 0.3% [95% CI, −0.4% to 0.9%]). Of 2472 children enrolled in the prospective cohort (1100 with acute otitis media; 705, group A streptococcal pharyngitis; and 667, acute sinusitis), 868 (35%) were prescribed broad-spectrum antibiotics. Broad-spectrum antibiotics were associated with a slightly worse child quality of life (score of 90.2 for broad-spectrum antibiotics vs 91.5 for narrow-spectrum antibiotics; score difference for full matched analysis, −1.4% [95% CI, −2.4% to −0.4%]) but not with other patient-centered outcomes. Broad-spectrum treatment was associated with a higher risk of adverse events documented by the clinician (3.7% for broad-spectrum antibiotics vs 2.7% for narrow-spectrum antibiotics; risk difference for full matched analysis, 1.1% [95% CI, 0.4% to 1.8%]) and reported by the patient (35.6% for broad-spectrum antibiotics vs 25.1% for narrow-spectrum antibiotics; risk difference for full matched analysis, 12.2% [95% CI, 7.3% to 17.2%]). Conclusions and Relevance Among children with acute respiratory tract infections, broad-spectrum antibiotics were not associated with better clinical or patient-centered outcomes compared with narrow-spectrum antibiotics, and were associated with higher rates of adverse events. These data support the use of narrow-spectrum antibiotics for most children with acute respiratory tract infections.
中文翻译:

广谱抗生素与窄谱抗生素与急性呼吸道感染儿童治疗失败、不良事件和生活质量的关系
重要性 急性呼吸道感染占儿童抗生素暴露的大部分,用于急性呼吸道感染的广谱抗生素处方正在增加。与窄谱治疗相比,尚不清楚广谱治疗是否与改善预后相关。目的比较广谱和窄谱抗生素治疗小儿急性呼吸道感染的疗效。设计、设置和参与者 一项回顾性队列研究评估临床结果,一项前瞻性队列研究评估 2015 年 1 月至 2015 年 1 月至 2015 年 6 个月至 12 岁之间被诊断患有急性呼吸道感染并开出口服抗生素的儿童的以患者为中心的结果2016 年 4 月,在宾夕法尼亚州和新泽西州的 31 个儿科初级保健机构网络中进行。对两个队列分别进行了分层和倾向评分匹配分析,以解释临床医生和患者水平特征的混杂因素。暴露广谱抗生素与窄谱抗生素。主要结局和措施 在回顾性队列中,主要结局是治疗失败和诊断后 14 天的不良事件。在前瞻性队列中,主要结局是生活质量、其他以患者为中心的结局以及患者报告的不良事件。结果 回顾性队列中的 30 159 名儿童(19 179 名急性中耳炎;6746 名 A 组链球菌性咽炎;4234 名急性鼻窦炎)中,有 4307 名(14%)服用了广谱抗生素,包括阿莫西林克拉维酸、头孢菌素和大环内酯类。广谱治疗与较低的治疗失败率无关(广谱抗生素为 3.4%,窄谱抗生素为 3.1%;完全匹配分析的风险差异为 0.3% [95% CI,-0.4% 至 0.9] %])。在纳入前瞻性队列的 2472 名儿童中(1100 名患有急性中耳炎;705 名患有 A 组链球菌性咽炎;667 名患有急性鼻窦炎),其中 868 名(35%)服用了广谱抗生素。广谱抗生素与儿童生活质量稍差相关(广谱抗生素得分为 90.2,窄谱抗生素得分为 91.5;完全匹配分析的得分差异为 -1.4% [95% CI,-2.4% 至−0.4%]),但不适用于其他以患者为中心的结果。广谱治疗与临床医生记录的较高不良事件风险相关(广谱抗生素为 3.7%,窄谱抗生素为 2.7%;完全匹配分析的风险差异为 1.1% [95% CI, 0.4%]至 1.8%])并由患者报告(广谱抗生素为 35.6%,窄谱抗生素为 25.1%;完全匹配分析的风险差异为 12.2% [95% CI,7.3% 至 17.2%])。结论和相关性 在患有急性呼吸道感染的儿童中,与窄谱抗生素相比,广谱抗生素与更好的临床或以患者为中心的结果无关,并且与较高的不良事件发生率相关。这些数据支持对大多数患有急性呼吸道感染的儿童使用窄谱抗生素。
更新日期:2017-12-19
中文翻译:

广谱抗生素与窄谱抗生素与急性呼吸道感染儿童治疗失败、不良事件和生活质量的关系
重要性 急性呼吸道感染占儿童抗生素暴露的大部分,用于急性呼吸道感染的广谱抗生素处方正在增加。与窄谱治疗相比,尚不清楚广谱治疗是否与改善预后相关。目的比较广谱和窄谱抗生素治疗小儿急性呼吸道感染的疗效。设计、设置和参与者 一项回顾性队列研究评估临床结果,一项前瞻性队列研究评估 2015 年 1 月至 2015 年 1 月至 2015 年 6 个月至 12 岁之间被诊断患有急性呼吸道感染并开出口服抗生素的儿童的以患者为中心的结果2016 年 4 月,在宾夕法尼亚州和新泽西州的 31 个儿科初级保健机构网络中进行。对两个队列分别进行了分层和倾向评分匹配分析,以解释临床医生和患者水平特征的混杂因素。暴露广谱抗生素与窄谱抗生素。主要结局和措施 在回顾性队列中,主要结局是治疗失败和诊断后 14 天的不良事件。在前瞻性队列中,主要结局是生活质量、其他以患者为中心的结局以及患者报告的不良事件。结果 回顾性队列中的 30 159 名儿童(19 179 名急性中耳炎;6746 名 A 组链球菌性咽炎;4234 名急性鼻窦炎)中,有 4307 名(14%)服用了广谱抗生素,包括阿莫西林克拉维酸、头孢菌素和大环内酯类。广谱治疗与较低的治疗失败率无关(广谱抗生素为 3.4%,窄谱抗生素为 3.1%;完全匹配分析的风险差异为 0.3% [95% CI,-0.4% 至 0.9] %])。在纳入前瞻性队列的 2472 名儿童中(1100 名患有急性中耳炎;705 名患有 A 组链球菌性咽炎;667 名患有急性鼻窦炎),其中 868 名(35%)服用了广谱抗生素。广谱抗生素与儿童生活质量稍差相关(广谱抗生素得分为 90.2,窄谱抗生素得分为 91.5;完全匹配分析的得分差异为 -1.4% [95% CI,-2.4% 至−0.4%]),但不适用于其他以患者为中心的结果。广谱治疗与临床医生记录的较高不良事件风险相关(广谱抗生素为 3.7%,窄谱抗生素为 2.7%;完全匹配分析的风险差异为 1.1% [95% CI, 0.4%]至 1.8%])并由患者报告(广谱抗生素为 35.6%,窄谱抗生素为 25.1%;完全匹配分析的风险差异为 12.2% [95% CI,7.3% 至 17.2%])。结论和相关性 在患有急性呼吸道感染的儿童中,与窄谱抗生素相比,广谱抗生素与更好的临床或以患者为中心的结果无关,并且与较高的不良事件发生率相关。这些数据支持对大多数患有急性呼吸道感染的儿童使用窄谱抗生素。


























 京公网安备 11010802027423号
京公网安备 11010802027423号