PLOS Neglected Tropical Diseases ( IF 3.8 ) Pub Date : 2017-11-20 , DOI: 10.1371/journal.pntd.0006095 Jipada Manomat , Saovanee Leelayoova , Lertwut Bualert , Peerapan Tan-ariya , Suradej Siripattanapipong , Mathirut Mungthin , Tawee Naaglor , Phunlerd Piyaraj
|
Background
Autochthonous cutaneous and visceral leishmaniasis (VL) caused by Leishmania martiniquensis and Leishmania siamensis have been considered emerging infectious diseases in Thailand. The disease burden is significantly underestimated, especially the prevalence of Leishmania infection among HIV-positive patients.
Methods
A cross-sectional study was conducted to determine the prevalence and risk factors associated with Leishmania infection among patients with HIV/AIDS living in Trang province, southern Thailand, between 2015 and 2016. Antibodies against Leishmania infection were assayed using the direct agglutination test (DAT). DNA of Leishmania was detected by ITS1-PCR using the buffy coat. Species of Leishmania were also identified.
Results
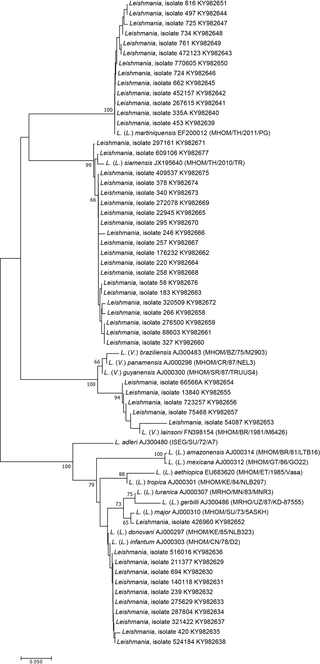
Of 724 participants, the prevalence of Leishmania infection was 25.1% (182/724) using either DAT and/or PCR assays. Seroprevalence of Leishmania infection was 18.5% (134/724), while Leishmania DNA detected by the PCR method was 8.4% (61/724). Of these, 24.9% (180/724) were asymptomatic, whereas 0.3% (2/724) were symptomatic VL and VL/CL (cutaneous leishmaniosis). At least five species were identified: L siamensis, L. martiniquensis, L. donovani complex, L. lainsoni, and L. major. Multivariate analysis showed that CD4+ levels <500 cells/μL and living in stilt houses were independently associated with Leishmania infection. Those who were PCR positive for Leishmania DNA were significantly associated with a detectable viral load, whereas non-injection drug use (NIDU) and CD4+ levels <500 cells/μL were potential risk factors of Leishmania seropositivity.
Conclusions
A magnitude of the prevalence of underreporting Leishmania infection among Thai patients with HIV was revealed in this study. Effective public health policy to prevent and control disease transmission is urgently needed.
中文翻译:

泰国南部董里省与利什曼原虫感染相关的患病率和危险因素
背景
在泰国,由利什曼原虫(Leishmania martiniquensis)和暹罗利什曼原虫(Leishmania siamensis)引起的皮肤和内脏利什曼原虫病(VL)被认为是新兴的传染病。疾病的负担被大大低估了,尤其是艾滋病毒抗体阳性患者中利什曼原虫感染的患病率。
方法
进行了一项横断面研究,以确定2015年至2016年之间居住在泰国南部董里省的HIV / AIDS患者中与利什曼原虫感染相关的患病率和危险因素。使用直接凝集试验(DAT)测定了针对利什曼原虫感染的抗体)。使用血沉棕黄层通过ITS1-PCR检测利什曼原虫的DNA 。还鉴定了利什曼原虫的种类。
结果
使用DAT和/或PCR分析,在724名参与者中,利什曼原虫感染的患病率为25.1%(182/724)。的血清流行病学利什曼原虫感染为18.5%(724分之134),而利什曼原虫DNA检测通过PCR法为8.4%(724分之61)。其中,24.9%(180/724)是无症状的,而0.3%(2/724)是有症状的VL和VL / CL(皮肤利什曼病)。至少有五个品种被确定:大号siamensis等,大号。martiniquensis,大号。原虫复杂,大号。lainsoni,和大号。专业的。多因素分析表明CD4+水平<500个细胞/μL且生活在高跷屋中与利什曼原虫感染独立相关。PCR检测为利什曼原虫DNA阳性的人与可检测的病毒载量显着相关,而未注射药物使用(NIDU)和CD4 +水平<500细胞/μL是利什曼原虫血清阳性的潜在危险因素。
结论
这项研究揭示了泰国艾滋病毒感染者报告不足的利什曼原虫感染的程度。迫切需要有效的公共卫生政策来预防和控制疾病的传播。



























 京公网安备 11010802027423号
京公网安备 11010802027423号