PLOS Medicine ( IF 15.8 ) Pub Date : 2017-11-14 , DOI: 10.1371/journal.pmed.1002434 Ingrid T. Katz , Richard Kaplan , Garrett Fitzmaurice , Dominick Leone , David R. Bangsberg , Linda-Gail Bekker , Catherine Orrell
|
Background
South Africa has undergone multiple expansions in antiretroviral therapy (ART) eligibility from an initial CD4+ threshold of ≤200 cells/μl to providing ART for all people living with HIV (PLWH) as of September 2016. We evaluated the association of programmatic changes in ART eligibility with loss from care, both prior to ART initiation and within the first 16 weeks of starting treatment, during a period of programmatic expansion to ART treatment at CD4+ ≤ 350 cells/μl.
Methods and findings
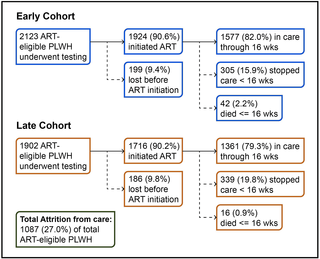
We performed a retrospective cohort study of 4,025 treatment-eligible, non-pregnant PLWH accessing care in a community health center in Gugulethu Township affiliated with the Desmond Tutu HIV Centre in Cape Town. The median age of participants was 34 years (IQR 28–41 years), almost 62% were female, and the median CD4+ count was 173 cells/μl (IQR 92–254 cells/μl). Participants were stratified into 2 cohorts: an early cohort, enrolled into care at the health center from 1 January 2009 to 31 August 2011, when guidelines mandated that ART initiation required CD4+ ≤ 200 cells/μl, pregnancy, advanced clinical symptoms (World Health Organization [WHO] stage 4), or comorbidity (active tuberculosis); and a later cohort, enrolled into care from 1 September 2011 to 31 December 2013, when the treatment threshold had been expanded to CD4+ ≤ 350 cells/μl. Demographic and clinical factors were compared before and after the policy change using chi-squared tests to identify potentially confounding covariates, and logistic regression models were used to estimate the risk of pre-treatment (pre-ART) loss from care and early loss within the first 16 weeks on treatment, adjusting for age, baseline CD4+, and WHO stage. Compared with participants in the later cohort, participants in the earlier cohort had significantly more advanced disease: median CD4+ 146 cells/μl versus 214 cells/μl (p < 0.001), 61.1% WHO stage 3/4 disease versus 42.8% (p < 0.001), and pre-ART mortality of 34.2% versus 16.7% (p < 0.001). In total, 385 ART-eligible PLWH (9.6%) failed to initiate ART, of whom 25.7% died before ever starting treatment. Of the 3,640 people who started treatment, 58 (1.6%) died within the first 16 weeks in care, and an additional 644 (17.7%) were lost from care within 16 weeks of starting ART. PLWH who did start treatment in the later cohort were significantly more likely to discontinue care in <16 weeks (19.8% versus 15.8%, p = 0.002). After controlling for baseline CD4+, WHO stage, and age, this effect remained significant (adjusted odds ratio [aOR] = 1.30, 95% CI 1.09–1.55). As such, it remains unclear if early attrition from care was due to a “healthy cohort” effect or to overcrowding as programs expanded to accommodate the broader guidelines for treatment. Our findings were limited by a lack of generalizability (given that these data were from a single high-volume site where testing and treatment were available) and an inability to formally investigate the effect of crowding on the main outcome.
Conclusions
Over one-quarter of this ART-eligible cohort did not achieve the long-term benefits of treatment due to early mortality, ART non-initiation, or early ART discontinuation. Those who started treatment in the later cohort appeared to be more likely to discontinue care early, and this outcome appeared to be independent of CD4+ count or WHO stage. Future interventions should focus on those most at risk for early loss from care as programs continue to expand in South Africa.
中文翻译:

南非开普敦的治疗指南和艾滋病毒感染者的早期护理损失:一项回顾性队列研究
背景
截至2016年9月,南非的抗逆转录病毒疗法(ART)资格已经历了多次扩展,从最初的CD4 +阈值≤200个细胞/微升开始,向所有HIV感染者提供抗逆转录病毒治疗(PLWH)。在CD4 + ≤350细胞/μl的程序性扩展至ART治疗的一段时间内,无论是在ART开始之前还是在开始治疗的前16周内,都有因失去治疗而获得ART的资格。
方法和发现
我们在开普敦Desmond Tutu HIV中心下属的Gugulethu镇的社区卫生中心对4025名符合治疗条件且未怀孕的PLWH获得护理进行了一项回顾性队列研究。受试者的中位年龄为34岁(IQR 28-41岁),女性几乎为62%,中位数CD4 +计数为173个细胞/微升(IQR 92-254细胞/微升)。参与者分为两个队列:一个早期队列,于2009年1月1日至2011年8月31日在健康中心就诊,当时指南要求抗病毒治疗必须CD4 +≤200细胞/μl,妊娠,晚期临床症状(世界卫生组织[WHO]第4阶段)或合并症(活动性肺结核);后来的一个研究小组于2011年9月1日至2013年12月31日加入治疗,当时治疗阈值已扩大至CD4 + ≤350细胞/μl。在政策变更前后使用卡方检验比较人口统计学和临床因素,以识别潜在的混杂变量,并使用逻辑回归模型来评估因护理造成的治疗前(ART)损失和患病早期损失的风险。治疗的前16周,根据年龄,基线CD4 +和WHO阶段进行调整。与晚期队列的参与者相比,早期队列的参与者患有明显更高的疾病:CD4中位数+ 146细胞/μl对214细胞/μl(p < 0.001),61.1%的WHO 3/4期疾病对42.8%(p < 0.001),ART前死亡率分别为34.2%和16.7%(p < 0.001)。总共385例符合ART要求的PLWH未能发起ART,其中25.7%的人在开始治疗前死亡。在开始治疗的3,640位患者中,有58位(1.6%)在接受护理的前16周内死亡,另有644位(17.7%)在开始接受抗逆转录病毒治疗后的16周内因护理而丧生。在后来的队列中开始治疗的PLWH在<16周内中断服务的可能性显着更高(19.8%对15.8%,p = 0.002)。控制基线CD4 +之后,世卫组织分期和年龄,这种影响仍然很显着(校正后的优势比[aOR] = 1.30,95%CI 1.09–1.55)。因此,目前尚不清楚早期减员是由于“健康人群”效应还是由于计划扩展以适应更广泛的治疗指南而人满为患。我们的发现受到缺乏普遍性的限制(假设这些数据来自可以进行测试和治疗的单个高容量站点),并且无法正式调查拥挤对主要结果的影响。
结论
由于早期死亡率,未开始抗逆转录病毒治疗或早期终止抗逆转录病毒治疗,这一符合抗逆转录病毒治疗的队列中有四分之一以上未获得长期治疗益处。在较晚的队列中开始治疗的患者似乎更有可能提前终止治疗,并且这一结果似乎与CD4 +计数或WHO阶段无关。随着南非计划的不断扩大,未来的干预措施应关注那些因早期护理而极易遭受风险的人。

























 京公网安备 11010802027423号
京公网安备 11010802027423号