JAMA Psychiatry ( IF 25.8 ) Pub Date : 2017-12-01 , DOI: 10.1001/jamapsychiatry.2017.3191 Fernando Pires Hartwig 1, 2 , Maria Carolina Borges 1, 2, 3 , Bernardo Lessa Horta 1 , Jack Bowden 2, 3 , George Davey Smith 2, 3
|
Importance Positive associations between inflammatory biomarkers and risk of psychiatric disorders, including schizophrenia, have been reported in observational studies. However, conventional observational studies are prone to bias, such as reverse causation and residual confounding, thus limiting our understanding of the effect (if any) of inflammatory biomarkers on schizophrenia risk.
Objective To evaluate whether inflammatory biomarkers have an effect on the risk of developing schizophrenia.
Design, Setting, and Participants Two-sample mendelian randomization study using genetic variants associated with inflammatory biomarkers as instrumental variables to improve inference. Summary association results from large consortia of candidate gene or genome-wide association studies, including several epidemiologic studies with different designs, were used. Gene-inflammatory biomarker associations were estimated in pooled samples ranging from 1645 to more than 80 000 individuals, while gene-schizophrenia associations were estimated in more than 30 000 cases and more than 45 000 ancestry-matched controls. In most studies included in the consortia, participants were of European ancestry, and the prevalence of men was approximately 50%. All studies were conducted in adults, with a wide age range (18 to 80 years).
Exposures Genetically elevated circulating levels of C-reactive protein (CRP), interleukin-1 receptor antagonist (IL-1Ra), and soluble interleukin-6 receptor (sIL-6R).
Main Outcomes and Measures Risk of developing schizophrenia. Individuals with schizophrenia or schizoaffective disorders were included as cases. Given that many studies contributed to the analyses, different diagnostic procedures were used.
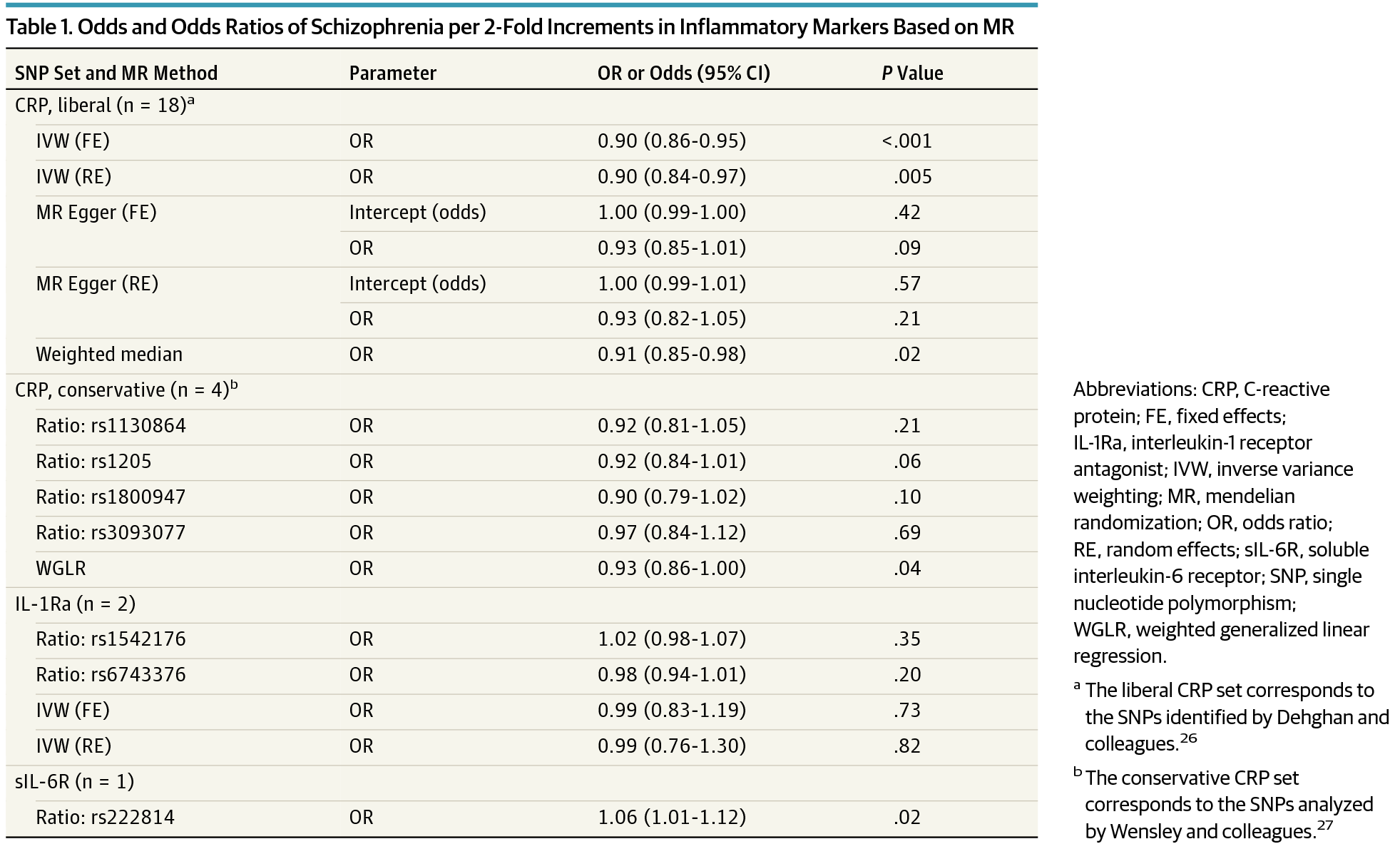
Results The pooled odds ratio estimate using 18 CRP genetic instruments was 0.90 (random effects 95% CI, 0.84-0.97; P = .005) per 2-fold increment in CRP levels; consistent results were obtained using different mendelian randomization methods and a more conservative set of instruments. The odds ratio for sIL-6R was 1.06 (95% CI, 1.01-1.12; P = .02) per 2-fold increment. Estimates for IL-1Ra were inconsistent among instruments, and pooled estimates were imprecise and centered on the null.
Conclusions and Relevance Under mendelian randomization assumptions, our findings suggest a protective effect of CRP and a risk-increasing effect of sIL-6R (potentially mediated at least in part by CRP) on schizophrenia risk. It is possible that such effects are a result of increased susceptibility to early life infection.
中文翻译:

炎症生物标志物和精神分裂症的风险一项 2 样本孟德尔随机化研究
重要性 观察性研究报告了炎症生物标志物与精神疾病(包括精神分裂症)风险之间的正相关。然而,传统的观察性研究容易出现偏见,例如反向因果关系和残余混杂,从而限制了我们对炎症生物标志物对精神分裂症风险的影响(如果有的话)的理解。
目的 评估炎症生物标志物是否对发生精神分裂症的风险有影响。
设计、设置和参与者 使用与炎症生物标志物相关的遗传变异作为工具变量来改进推理的两样本孟德尔随机化研究。使用了来自候选基因或全基因组关联研究的大型联盟的总结关联结果,包括具有不同设计的几项流行病学研究。在 1645 到 80 000 多人的汇总样本中估计了基因炎症生物标志物关联,而在超过 30 000 例病例和超过 45 000 名血统匹配的对照中估计了基因-精神分裂症关联。在该联盟的大多数研究中,参与者都是欧洲血统,男性的患病率约为 50%。所有研究均在成年人中进行,年龄范围很广(18 至 80 岁)。
暴露 C 反应蛋白 (CRP)、白细胞介素 1 受体拮抗剂 (IL-1Ra) 和可溶性白细胞介素 6 受体 (sIL-6R) 的遗传升高的循环水平。
主要结果和措施 发展精神分裂症的风险。患有精神分裂症或分裂情感障碍的个体被列为病例。鉴于许多研究有助于分析,因此使用了不同的诊断程序。
结果 使用 18 种 CRP 遗传工具的汇总优势比估计值为 0.90(随机效应 95% CI,0.84-0.97;P = 0.005)每增加 2 倍 CRP 水平;使用不同的孟德尔随机化方法和一组更保守的工具获得了一致的结果。sIL-6R 的优势比为 1.06(95% CI,1.01-1.12;P = .02)每 2 倍增量。仪器之间对 IL-1Ra 的估计值不一致,汇总估计值不精确且以零为中心。
结论和相关性 在孟德尔随机化假设下,我们的研究结果表明 CRP 对精神分裂症风险具有保护作用和 sIL-6R(可能至少部分由 CRP 介导)的风险增加作用。这种影响可能是生命早期感染易感性增加的结果。



























 京公网安备 11010802027423号
京公网安备 11010802027423号