当前位置:
X-MOL 学术
›
Adv. Healthcare Mater.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
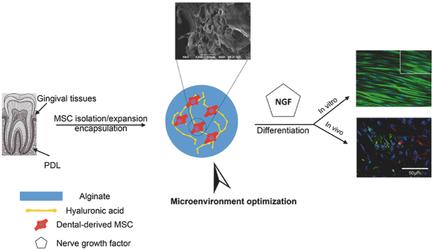
Human Periodontal Ligament‐ and Gingiva‐derived Mesenchymal Stem Cells Promote Nerve Regeneration When Encapsulated in Alginate/Hyaluronic Acid 3D Scaffold
Advanced Healthcare Materials ( IF 10.0 ) Pub Date : 2017-10-27 , DOI: 10.1002/adhm.201700670 Sahar Ansari 1 , Ivana M. Diniz 2 , Chider Chen 3 , Patricia Sarrion 1 , Ali Tamayol 4 , Benjamin M. Wu 1 , Alireza Moshaverinia 1
Advanced Healthcare Materials ( IF 10.0 ) Pub Date : 2017-10-27 , DOI: 10.1002/adhm.201700670 Sahar Ansari 1 , Ivana M. Diniz 2 , Chider Chen 3 , Patricia Sarrion 1 , Ali Tamayol 4 , Benjamin M. Wu 1 , Alireza Moshaverinia 1
Affiliation
|
Repair or regeneration of damaged nerves is still a challenging clinical task in reconstructive surgeries and regenerative medicine. Here, it is demonstrated that periodontal ligament stem cells (PDLSCs) and gingival mesenchymal stem cells (GMSCs) isolated from adult human periodontal and gingival tissues assume neuronal phenotype in vitro and in vivo via a subcutaneous transplantation model in nude mice. PDLSCs and GMSCs are encapsulated in a 3D scaffold based on alginate and hyaluronic acid hydrogels capable of sustained release of human nerve growth factor (NGF). The elasticity of the hydrogels affects the proliferation and differentiation of encapsulated MSCs within scaffolds. Moreover, it is observed that PDLSCs and GMSCs are stained positive for βIII‐tubulin, while exhibiting high levels of gene expression related to neurogenic differentiation (βIII‐tubulin and glial fibrillary acidic protein) via quantitative polymerase chain reaction (qPCR). Western blot analysis shows the importance of elasticity of the matrix and the presence of NGF in the neurogenic differentiation of encapsulated MSCs. In vivo, immunofluorescence staining for neurogenic specific protein markers confirms islands of dense positively stained structures inside transplanted hydrogels. As far as it is known, this study is the first demonstration of the application of PDLSCs and GMSCs as promising cell therapy candidates for nerve regeneration.
中文翻译:

当封装在藻酸盐/透明质酸3D支架中时,人类牙周膜和牙龈间质干细胞可促进神经再生。
在重建手术和再生医学中,受损神经的修复或再生仍然是一项具有挑战性的临床任务。在这里,证明了从成年人牙周和牙龈组织分离的牙周膜干细胞(PDLSC)和牙龈间充质干细胞(GMSC)在裸鼠中通过皮下移植模型在体内和体外呈现神经元表型。PDLSC和GMSC被封装在基于藻酸盐和透明质酸水凝胶的3D支架中,该凝胶能够持续释放人神经生长因子(NGF)。水凝胶的弹性影响支架内封装的MSC的增殖和分化。此外,我们发现PDLSC和GMSC对βIII-微管蛋白染色呈阳性,同时通过定量聚合酶链反应(qPCR)表现出与神经源性分化相关的高水平基因表达(βIII-微管蛋白和神经胶质纤维酸性蛋白)。蛋白质印迹分析显示了基质弹性和NGF的存在在封装的MSC的神经源性分化中的重要性。在体内,对神经源性特定蛋白标记物的免疫荧光染色证实了移植水凝胶内部密集的正染色结构岛。据了解,这项研究首次证明了PDLSCs和GMSCs作为有希望的神经再生细胞治疗候选物的应用。蛋白质印迹分析显示了基质弹性和NGF的存在在封装的MSC的神经源性分化中的重要性。在体内,对神经源性特定蛋白标记物的免疫荧光染色证实了移植水凝胶内部密集的正染色结构岛。据了解,这项研究首次证明了PDLSCs和GMSCs作为有希望的神经再生细胞治疗候选物的应用。蛋白质印迹分析显示了基质弹性和NGF的存在在封装的MSC的神经源性分化中的重要性。在体内,对神经源性特定蛋白标记物的免疫荧光染色证实了移植水凝胶内部密集的正染色结构岛。据了解,这项研究首次证明了PDLSCs和GMSCs作为有希望的神经再生细胞治疗候选物的应用。
更新日期:2017-10-27
中文翻译:

当封装在藻酸盐/透明质酸3D支架中时,人类牙周膜和牙龈间质干细胞可促进神经再生。
在重建手术和再生医学中,受损神经的修复或再生仍然是一项具有挑战性的临床任务。在这里,证明了从成年人牙周和牙龈组织分离的牙周膜干细胞(PDLSC)和牙龈间充质干细胞(GMSC)在裸鼠中通过皮下移植模型在体内和体外呈现神经元表型。PDLSC和GMSC被封装在基于藻酸盐和透明质酸水凝胶的3D支架中,该凝胶能够持续释放人神经生长因子(NGF)。水凝胶的弹性影响支架内封装的MSC的增殖和分化。此外,我们发现PDLSC和GMSC对βIII-微管蛋白染色呈阳性,同时通过定量聚合酶链反应(qPCR)表现出与神经源性分化相关的高水平基因表达(βIII-微管蛋白和神经胶质纤维酸性蛋白)。蛋白质印迹分析显示了基质弹性和NGF的存在在封装的MSC的神经源性分化中的重要性。在体内,对神经源性特定蛋白标记物的免疫荧光染色证实了移植水凝胶内部密集的正染色结构岛。据了解,这项研究首次证明了PDLSCs和GMSCs作为有希望的神经再生细胞治疗候选物的应用。蛋白质印迹分析显示了基质弹性和NGF的存在在封装的MSC的神经源性分化中的重要性。在体内,对神经源性特定蛋白标记物的免疫荧光染色证实了移植水凝胶内部密集的正染色结构岛。据了解,这项研究首次证明了PDLSCs和GMSCs作为有希望的神经再生细胞治疗候选物的应用。蛋白质印迹分析显示了基质弹性和NGF的存在在封装的MSC的神经源性分化中的重要性。在体内,对神经源性特定蛋白标记物的免疫荧光染色证实了移植水凝胶内部密集的正染色结构岛。据了解,这项研究首次证明了PDLSCs和GMSCs作为有希望的神经再生细胞治疗候选物的应用。



























 京公网安备 11010802027423号
京公网安备 11010802027423号