Journal of Allergy and Clinical Immunology ( IF 14.2 ) Pub Date : 2017-10-23 , DOI: 10.1016/j.jaci.2017.08.039 Brecht Steelant , Sven F. Seys , Laura Van Gerven , Matthias Van Woensel , Ricard Farré , Paulina Wawrzyniak , Inge Kortekaas Krohn , Dominique M. Bullens , Karel Talavera , Ulrike Raap , Louis Boon , Cezmi A. Akdis , Guy Boeckxstaens , Jan L. Ceuppens , Peter W. Hellings
|
Background
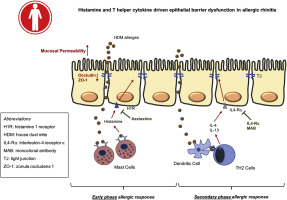
Allergic rhinitis (AR) is characterized by mucosal inflammation, driven by activated immune cells. Mast cells and TH2 cells might decrease epithelial barrier integrity in AR, maintaining a leaky epithelial barrier.
Objective
We sought to investigate the role of histamine and TH2 cells in driving epithelial barrier dysfunction in AR.
Methods
Air-liquid interface cultures of primary nasal epithelial cells were used to measure transepithelial electrical resistance, paracellular flux of fluorescein isothiocyanate-dextran 4 kDa, and mRNA expression of tight junctions. Nasal secretions were collected from healthy control subjects, AR patients, and idiopathic rhinitis patients and were tested in vitro. In addition, the effect of activated TH1 and TH2 cells, mast cells, and neurons was tested in vitro. The effect of IL-4, IL-13, IFN-γ, and TNF-α on mucosal permeability was tested in vivo.
Results
Histamine as well as nasal secretions of AR but not idiopathic rhinitis patients rapidly decreased epithelial barrier integrity in vitro. Pretreatment with histamine receptor-1 antagonist, azelastine prevented the early effect of nasal secretions of AR patients on epithelial integrity. Supernatant of activated TH1 and TH2 cells impaired epithelial integrity, while treatment with anti-TNF-α or anti-IL-4Rα monoclonal antibodies restored the TH1- and TH2-induced epithelial barrier dysfunction, respectively. IL-4, IFN-γ, and TNF-α enhanced mucosal permeability in mice. Antagonizing IL-4 prevented mucosal barrier disruption and tight junction downregulation in a mouse model of house dust mite allergic airway inflammation.
Conclusions
Our data indicate a key role for allergic inflammatory mediators in modulating nasal epithelial barrier integrity in the pathophysiology in AR.
中文翻译:

组胺和T辅助细胞因子驱动的变应性鼻炎中上皮屏障功能障碍
背景
过敏性鼻炎(AR)的特征是由活化的免疫细胞驱动的粘膜炎症。肥大细胞和T H 2细胞可能会降低AR中的上皮屏障完整性,从而维持渗漏的上皮屏障。
客观的
我们试图探讨组胺和T的作用^ h 2个细胞中的AR驱动上皮屏障功能障碍。
方法
鼻上皮细胞的气液界面培养用于测量跨上皮电阻,异硫氰酸荧光素-葡聚糖4 kDa的细胞旁通量以及紧密连接的mRNA表达。从健康对照受试者,AR患者和特发性鼻炎患者收集鼻分泌物,并进行体外测试。此外,活化的T的效果ħ 1和T ħ 2个细胞,肥大细胞和神经元中测试在体外。在体内测试了IL-4,IL-13,IFN-γ和TNF-α对粘膜通透性的作用。
结果
组胺以及AR的鼻腔分泌物而非特发性鼻炎患者在体外迅速降低上皮屏障的完整性。用组胺受体1拮抗剂预处理,氮卓斯汀可防止AR患者鼻分泌物对上皮完整性的早期影响。活化的T H 1和T H 2细胞的上清液会损害上皮完整性,而抗TNF-α或抗IL-4Rα单克隆抗体的治疗可恢复T H 1和T H2型诱导的上皮屏障功能障碍。IL-4,IFN-γ和TNF-α增强了小鼠的粘膜通透性。在小鼠尘螨过敏性气道炎症小鼠模型中,拮抗IL-4可以防止粘膜屏障破坏和紧密连接下调。
结论
我们的数据表明,过敏性炎症介质在调节AR的病理生理过程中在调节鼻黏膜上皮屏障完整性方面起着关键作用。



























 京公网安备 11010802027423号
京公网安备 11010802027423号