PLOS Medicine ( IF 15.8 ) Pub Date : 2017-10-31 , DOI: 10.1371/journal.pmed.1002412 Terry P. Haines , Kelly-Ann Bowles , Deb Mitchell , Lisa O’Brien , Donna Markham , Samantha Plumb , Kerry May , Kathleen Philip , Romi Haas , Mitchell N. Sarkies , Marcelle Ghaly , Melina Shackell , Timothy Chiu , Steven McPhail , Fiona McDermott , Elizabeth H. Skinner
|
Background
Disinvestment (removal, reduction, or reallocation) of routinely provided health services can be difficult when there is little published evidence examining whether the services are effective or not. Evidence is required to understand if removing these services produces outcomes that are inferior to keeping such services in place. However, organisational imperatives, such as budget cuts, may force healthcare providers to disinvest from these services before the required evidence becomes available. There are presently no experimental studies examining the effectiveness of allied health services (e.g., physical therapy, occupational therapy, and social work) provided on weekends across acute medical and surgical hospital wards, despite these services being routinely provided internationally. The aim of this study was to understand the impact of removing weekend allied health services from acute medical and surgical wards using a disinvestment-specific non-inferiority research design.
Methods and findings
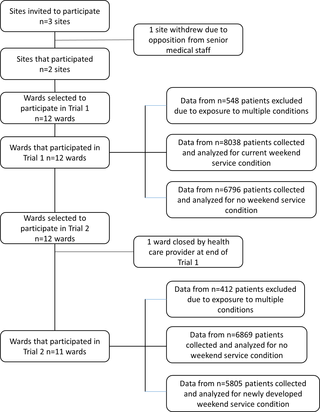
We conducted 2 stepped-wedge cluster randomised controlled trials between 1 February 2014 and 30 April 2015 among patients on 12 acute medical or surgical hospital wards spread across 2 hospitals. The hospitals involved were 2 metropolitan teaching hospitals in Melbourne, Australia. Data from n = 14,834 patients were collected for inclusion in Trial 1, and n = 12,674 in Trial 2. Trial 1 was a disinvestment-specific non-inferiority stepped-wedge trial where the ‘current’ weekend allied health service was incrementally removed from participating wards each calendar month, in a random order, while Trial 2 used a conventional non-inferiority stepped-wedge design, where a ‘newly developed’ service was incrementally reinstated on the same wards as in Trial 1. Primary outcome measures were patient length of stay (proportion staying longer than expected and mean length of stay), the proportion of patients experiencing any adverse event, and the proportion with an unplanned readmission within 28 days of discharge. The ‘no weekend allied health service’ condition was considered to be not inferior if the 95% CIs of the differences between this condition and the condition with weekend allied health service delivery were below a 2% increase in the proportion of patients who stayed in hospital longer than expected, a 2% increase in the proportion who had an unplanned readmission within 28 days, a 2% increase in the proportion who had any adverse event, and a 1-day increase in the mean length of stay. The current weekend allied health service included physical therapy, occupational therapy, speech therapy, dietetics, social work, and allied health assistant services in line with usual care at the participating sites. The newly developed weekend allied health service allowed managers at each site to reprioritise tasks being performed and the balance of hours provided by each professional group and on which days they were provided. Analyses conducted on an intention-to-treat basis demonstrated that there was no estimated effect size difference between groups in the proportion of patients staying longer than expected (weekend versus no weekend; estimated effect size difference [95% CI], p-value) in Trial 1 (0.40 versus 0.38; estimated effect size difference 0.01 [−0.01 to 0.04], p = 0.31, CI was both above and below non-inferiority margin), but the proportion staying longer than expected was greater with the newly developed service compared to its no weekend service control condition (0.39 versus 0.40; estimated effect size difference 0.02 [0.01 to 0.04], p = 0.04, CI was completely below non-inferiority margin) in Trial 2. Trial 1 and 2 findings were discordant for the mean length of stay outcome (Trial 1: 5.5 versus 6.3 days; estimated effect size difference 1.3 days [0.9 to 1.8], p < 0.001, CI was both above and below non-inferiority margin; Trial 2: 5.9 versus 5.0 days; estimated effect size difference −1.6 days [−2.0 to −1.1], p < 0.001, CI was completely below non-inferiority margin). There was no difference between conditions for the proportion who had an unplanned readmission within 28 days in either trial (Trial 1: 0.01 [−0.01 to 0.03], p = 0.18, CI was both above and below non-inferiority margin; Trial 2: −0.01 [−0.02 to 0.01], p = 0.62, CI completely below non-inferiority margin). There was no difference between conditions in the proportion of patients who experienced any adverse event in Trial 1 (0.01 [−0.01 to 0.03], p = 0.33, CI was both above and below non-inferiority margin), but a lower proportion of patients had an adverse event in Trial 2 when exposed to the no weekend allied health condition (−0.03 [−0.05 to −0.004], p = 0.02, CI completely below non-inferiority margin). Limitations of this research were that 1 of the trial wards was closed by the healthcare provider after Trial 1 and could not be included in Trial 2, and that both withdrawing the current weekend allied health service model and installing a new one may have led to an accommodation period for staff to adapt to the new service settings. Stepped-wedge trials are potentially susceptible to bias from naturally occurring change over time at the service level; however, this was adjusted for in our analyses.
Conclusions
In Trial 1, criteria to say that the no weekend allied health condition was non-inferior to current weekend allied health condition were not met, while neither the no weekend nor current weekend allied health condition demonstrated superiority. In Trial 2, the no weekend allied health condition was non-inferior to the newly developed weekend allied health condition across all primary outcomes, and superior for the outcomes proportion of patients staying longer than expected, proportion experiencing any adverse event, and mean length of stay.
Trial registration
Australian New Zealand Clinical Trials Registry ACTRN12613001231730 and ACTRN12613001361796
中文翻译:

从周末相关医疗服务中撤资对急性医疗和外科病房的影响:2步楔形聚类随机对照试验
背景
当很少有公开证据证明服务是否有效时,很难对常规提供的医疗服务进行投资(撤除,削减或重新分配)。需要证据来了解删除这些服务是否产生的效果不如将这些服务保持在适当的位置。但是,诸如削减预算之类的组织要求可能会迫使医疗保健提供者在获得所需证据之前放弃对这些服务的投资。尽管在国际上常规提供这些服务,但目前还没有实验研究在周末在急性医学和外科医院病房中提供相关健康服务(例如物理治疗,职业治疗和社会工作)的有效性。
方法和发现
我们在2014年2月1日至2015年4月30日之间,对分布在2家医院的12个急性内科或外科医院病房的患者进行了2项阶梯楔类随机对照试验。所涉及的医院是澳大利亚墨尔本的2家大都会教学医院。收集了来自n = 14,834例患者的数据以纳入试验1,其中n =如果“无周末专职医疗服务”条件与接受周末专职医疗服务的条件之间的差异的95%CI低于住院患者比例增加了2%,则认为“无周末专职医疗服务”条件并不逊色比预期更长的时间,计划外重新入院的比例在28天内增加了2%,有不良事件的比例增加了2%,平均住院时间增加了1天。当前周末的联合健康服务包括物理治疗,职业治疗,言语治疗,饮食学,社会工作以及与参与场所的常规护理相符的联合健康助手服务。新近开发的周末专职医疗服务使每个站点的经理可以优先执行正在执行的任务,并优先考虑每个专业小组提供的工作时间以及在工作日提供的时间。在意向性治疗的基础上进行的分析表明,在两组患者中,住院时间长于预期的比例没有估计的效应量差异(周末与非周末;估计的效应量差异[95%CI],试验1中的p值(0.40对0.38;估计的效应大小差异0.01 [-0.01至0.04],p = 0.31,CI均在非劣效性边际之上和之下),但与预期相比,停留时间长于预期的比例更大在试验2中,新开发的服务与其无周末服务控制条件(0.39对0.40;估计的效应大小差异0.02 [0.01至0.04],p = 0.04,CI完全低于非自卑裕度)相比,试验1和2的发现与平均住院时间长短不一致(试验1:5.5天与6.3天;估计的影响大小差异1.3天[0.9到1.8],p <0.001,CI低于和低于非劣质性边缘;试用2:5.9天和5.0天;估计效应大小差异为-1.6天[-2.0至-1.1],p < 0.001,CI完全低于非劣效性边缘)。在两项试验中,计划外入院的比例在28天之内的条件之间没有差异(试验1:0.01 [-0.01至0.03],p = 0.18,CI高于和低于非劣效性边缘;试验2: -0.01 [-0.02至0.01],p = 0.62,CI完全低于非劣效性余量)。在试验1中,经历任何不良事件的患者所占的比例在条件之间没有差异(0.01 [-0.01至0.03],p =0.33,CI均高于和低于非劣质性差,但在试验2中,在没有周末相关健康状况的情况下,有较低比例的患者发生不良事件(-0.03 [-0.05至-0.004],p = 0.02 ,CI完全低于非劣质性边缘)。这项研究的局限性在于,试验室中的1个在1号试验后被医疗服务提供者关闭,不能纳入2号试验,并且撤回当前周末的联合医疗服务模式并安装新的模型可能导致了员工的住宿时间以适应新的服务设置。在服务级别上,逐步楔入试验可能会随时间自然变化而产生偏差;但是,在我们的分析中对此进行了调整。
结论
在试验1中,没有满足这样的标准,即没有周末相关健康状况不逊于当前周末相关健康状况,而没有周末或当前周末相关健康状况均未显示出优越性。在试验2中,在所有主要结局中,无周末专职健康状况均不逊于新开发的周末专职健康状况,并且其结局指标是:住院时间长于预期,经历任何不良事件的比例以及平均病程停留。
试用注册
澳大利亚新西兰临床试验注册中心ACTRN12613001231730和ACTRN12613001361796



























 京公网安备 11010802027423号
京公网安备 11010802027423号