当前位置:
X-MOL 学术
›
JAMA Pediatr.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Effectiveness of β-Lactam Monotherapy vs Macrolide Combination Therapy for Children Hospitalized With Pneumonia
JAMA Pediatrics ( IF 26.1 ) Pub Date : 2017-12-01 , DOI: 10.1001/jamapediatrics.2017.3225 Derek J. Williams 1 , Kathryn M. Edwards 2 , Wesley H. Self 3 , Yuwei Zhu 4 , Sandra R. Arnold 5 , Jonathan A. McCullers 5 , Krow Ampofo 6 , Andrew T. Pavia 7 , Evan J. Anderson 8 , Lauri A. Hicks 9 , Anna M. Bramley 9 , Seema Jain 9 , Carlos G. Grijalva 10
JAMA Pediatrics ( IF 26.1 ) Pub Date : 2017-12-01 , DOI: 10.1001/jamapediatrics.2017.3225 Derek J. Williams 1 , Kathryn M. Edwards 2 , Wesley H. Self 3 , Yuwei Zhu 4 , Sandra R. Arnold 5 , Jonathan A. McCullers 5 , Krow Ampofo 6 , Andrew T. Pavia 7 , Evan J. Anderson 8 , Lauri A. Hicks 9 , Anna M. Bramley 9 , Seema Jain 9 , Carlos G. Grijalva 10
Affiliation
|
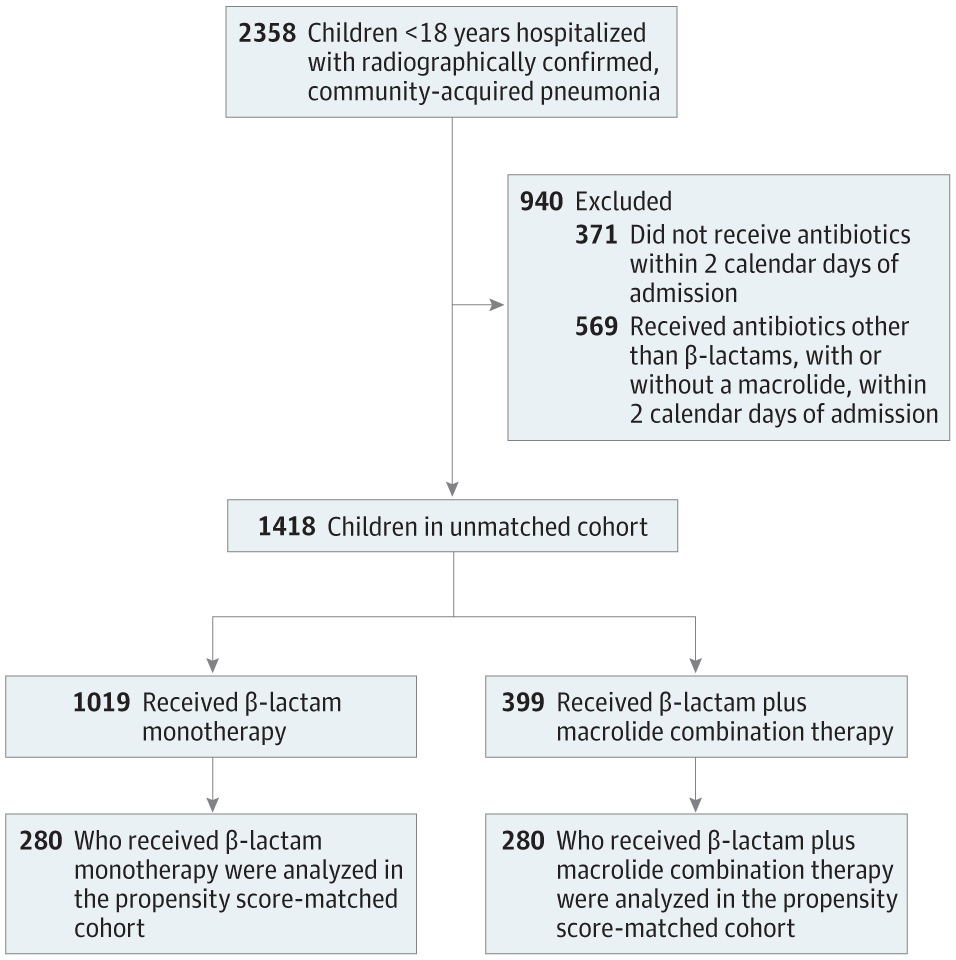
Importance &bgr;-Lactam monotherapy and &bgr;-lactam plus macrolide combination therapy are both common empirical treatment strategies for children hospitalized with pneumonia, but few studies have evaluated the effectiveness of these 2 treatment approaches. Objective To compare the effectiveness of &bgr;-lactam monotherapy vs &bgr;-lactam plus macrolide combination therapy among a cohort of children hospitalized with pneumonia. Design, Setting, and Participants We analyzed data from the Etiology of Pneumonia in the Community Study, a multicenter, prospective, population-based study of community-acquired pneumonia hospitalizations conducted from January 1, 2010, to June 30, 2012, in 3 children’s hospitals in Nashville, Tennessee; Memphis, Tennessee; and Salt Lake City, Utah. The study included all children (up to 18 years of age) who were hospitalized with radiographically confirmed pneumonia and who received &bgr;-lactam monotherapy or &bgr;-lactam plus macrolide combination therapy. Data analysis was completed in April 2017. Main Outcomes and Measures We defined the referent as &bgr;-lactam monotherapy, including exclusive use of an oral or parenteral second- or third-generation cephalosporin, penicillin, ampicillin, ampicillin-sulbactam, amoxicillin, or amoxicillin-clavulanate. Use of a &bgr;-lactam plus an oral or parenteral macrolide (azithromycin or clarithromycin) served as the comparison group. We modeled the association between these groups and patients’ length of stay using multivariable Cox proportional hazards regression. Covariates included demographic, clinical, and radiographic variables. We further evaluated length of stay in a cohort matched by propensity to receive combination therapy. Logistic regression was used to evaluate secondary outcomes in the unmatched cohort, including intensive care admission, rehospitalizations, and self-reported recovery at follow-up. Results Our study included 1418 children (693 girls and 725 boys) with a median age of 27 months (interquartile range, 12-69 months). This cohort was 60.1% of the 2358 children enrolled in the Etiology of Pneumonia in the Community Study with radiographically confirmed pneumonia in the study period; 1019 (71.9%) received &bgr;-lactam monotherapy and 399 (28.1%) received &bgr;-lactam plus macrolide combination therapy. In the unmatched cohort, there was no statistically significant difference in length of hospital stay between children receiving &bgr;-lactam monotherapy and combination therapy (median, 55 vs 59 hours; adjusted hazard ratio, 0.87; 95% CI, 0.74-1.01). The propensity-matched cohort (n = 560, 39.5%) showed similar results. There were also no significant differences between treatment groups for the secondary outcomes. Conclusions and Relevance Empirical macrolide combination therapy conferred no benefit over &bgr;-lactam monotherapy for children hospitalized with community-acquired pneumonia. The results of this study elicit questions about the routine empirical use of macrolide combination therapy in this population.
中文翻译:

β-内酰胺单药治疗与大环内酯联合治疗对肺炎住院患儿的疗效
重要性 &bgr;-内酰胺单药治疗和 &bgr;-内酰胺加大环内酯联合治疗都是肺炎住院患儿常见的经验性治疗策略,但很少有研究评估这两种治疗方法的有效性。目的比较&bgr;-内酰胺单药与&bgr;-内酰胺加大环内酯联合治疗在肺炎住院儿童队列中的疗效。设计、设置和参与者 我们分析了社区研究中肺炎病因学的数据,这是一项多中心、前瞻性、基于人群的研究,于 2010 年 1 月 1 日至 2012 年 6 月 30 日在 3 名儿童中进行了社区获得性肺炎住院治疗。田纳西州纳什维尔的医院;田纳西州孟菲斯;和犹他州盐湖城。该研究包括所有因影像学确诊肺炎住院并接受 β-内酰胺单药治疗或 β-内酰胺加大环内酯联合治疗的儿童(不超过 18 岁)。数据分析于 2017 年 4 月完成。 主要结果和措施 我们将参照物定义为 &bgr;-内酰胺单药治疗,包括单独使用口服或肠外二代或三代头孢菌素、青霉素、氨苄西林、氨苄西林-舒巴坦、阿莫西林或阿莫西林-克拉维酸。使用β-内酰胺加口服或肠胃外大环内酯(阿奇霉素或克拉霉素)作为对照组。我们使用多变量 Cox 比例风险回归模拟了这些组与患者住院时间之间的关联。协变量包括人口统计学、临床、和放射学变量。我们进一步评估了与接受联合治疗的倾向相匹配的队列中的住院时间。Logistic回归用于评估未匹配队列的次要结局,包括重症监护入院、再住院和随访时自我报告的恢复情况。结果 我们的研究包括 1418 名儿童(693 名女孩和 725 名男孩),平均年龄为 27 个月(四分位距,12-69 个月)。该队列是在社区研究中参加肺炎病因学研究的 2358 名儿童中的 60.1% 在研究期间患有放射学证实的肺炎;1019 名 (71.9%) 接受了 &bgr;-内酰胺单药治疗,399 名 (28.1%) 接受了 &bgr;-内酰胺加大环内酯联合治疗。在无与伦比的队列中,接受β-内酰胺单药治疗和联合治疗的儿童住院时间没有统计学显着差异(中位数,55 小时 vs 59 小时;调整后的风险比,0.87;95% CI,0.74-1.01)。倾向匹配队列(n = 560, 39.5%)显示出相似的结果。在次要结果方面,治疗组之间也没有显着差异。结论和相关性 对于社区获得性肺炎住院儿童,经验性大环内酯类联合治疗与 β-内酰胺单药治疗相比没有任何益处。这项研究的结果引发了有关在该人群中常规经验性使用大环内酯联合治疗的问题。倾向匹配队列(n = 560, 39.5%)显示出相似的结果。在次要结果方面,治疗组之间也没有显着差异。结论和相关性 对于社区获得性肺炎住院儿童,经验性大环内酯类联合治疗与 β-内酰胺单药治疗相比没有任何益处。这项研究的结果引发了有关在该人群中常规经验性使用大环内酯联合治疗的问题。倾向匹配队列(n = 560, 39.5%)显示出相似的结果。在次要结果方面,治疗组之间也没有显着差异。结论和相关性 对于社区获得性肺炎住院儿童,经验性大环内酯类联合治疗与 β-内酰胺单药治疗相比没有任何益处。这项研究的结果引发了有关在该人群中常规经验性使用大环内酯联合治疗的问题。
更新日期:2017-12-01
中文翻译:

β-内酰胺单药治疗与大环内酯联合治疗对肺炎住院患儿的疗效
重要性 &bgr;-内酰胺单药治疗和 &bgr;-内酰胺加大环内酯联合治疗都是肺炎住院患儿常见的经验性治疗策略,但很少有研究评估这两种治疗方法的有效性。目的比较&bgr;-内酰胺单药与&bgr;-内酰胺加大环内酯联合治疗在肺炎住院儿童队列中的疗效。设计、设置和参与者 我们分析了社区研究中肺炎病因学的数据,这是一项多中心、前瞻性、基于人群的研究,于 2010 年 1 月 1 日至 2012 年 6 月 30 日在 3 名儿童中进行了社区获得性肺炎住院治疗。田纳西州纳什维尔的医院;田纳西州孟菲斯;和犹他州盐湖城。该研究包括所有因影像学确诊肺炎住院并接受 β-内酰胺单药治疗或 β-内酰胺加大环内酯联合治疗的儿童(不超过 18 岁)。数据分析于 2017 年 4 月完成。 主要结果和措施 我们将参照物定义为 &bgr;-内酰胺单药治疗,包括单独使用口服或肠外二代或三代头孢菌素、青霉素、氨苄西林、氨苄西林-舒巴坦、阿莫西林或阿莫西林-克拉维酸。使用β-内酰胺加口服或肠胃外大环内酯(阿奇霉素或克拉霉素)作为对照组。我们使用多变量 Cox 比例风险回归模拟了这些组与患者住院时间之间的关联。协变量包括人口统计学、临床、和放射学变量。我们进一步评估了与接受联合治疗的倾向相匹配的队列中的住院时间。Logistic回归用于评估未匹配队列的次要结局,包括重症监护入院、再住院和随访时自我报告的恢复情况。结果 我们的研究包括 1418 名儿童(693 名女孩和 725 名男孩),平均年龄为 27 个月(四分位距,12-69 个月)。该队列是在社区研究中参加肺炎病因学研究的 2358 名儿童中的 60.1% 在研究期间患有放射学证实的肺炎;1019 名 (71.9%) 接受了 &bgr;-内酰胺单药治疗,399 名 (28.1%) 接受了 &bgr;-内酰胺加大环内酯联合治疗。在无与伦比的队列中,接受β-内酰胺单药治疗和联合治疗的儿童住院时间没有统计学显着差异(中位数,55 小时 vs 59 小时;调整后的风险比,0.87;95% CI,0.74-1.01)。倾向匹配队列(n = 560, 39.5%)显示出相似的结果。在次要结果方面,治疗组之间也没有显着差异。结论和相关性 对于社区获得性肺炎住院儿童,经验性大环内酯类联合治疗与 β-内酰胺单药治疗相比没有任何益处。这项研究的结果引发了有关在该人群中常规经验性使用大环内酯联合治疗的问题。倾向匹配队列(n = 560, 39.5%)显示出相似的结果。在次要结果方面,治疗组之间也没有显着差异。结论和相关性 对于社区获得性肺炎住院儿童,经验性大环内酯类联合治疗与 β-内酰胺单药治疗相比没有任何益处。这项研究的结果引发了有关在该人群中常规经验性使用大环内酯联合治疗的问题。倾向匹配队列(n = 560, 39.5%)显示出相似的结果。在次要结果方面,治疗组之间也没有显着差异。结论和相关性 对于社区获得性肺炎住院儿童,经验性大环内酯类联合治疗与 β-内酰胺单药治疗相比没有任何益处。这项研究的结果引发了有关在该人群中常规经验性使用大环内酯联合治疗的问题。



























 京公网安备 11010802027423号
京公网安备 11010802027423号