当前位置:
X-MOL 学术
›
J. Allergy Clin. Immunol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
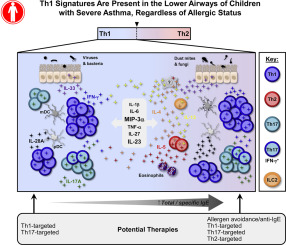
TH1 signatures are present in the lower airways of children with severe asthma, regardless of allergic status.
Journal of Allergy and Clinical Immunology ( IF 14.2 ) Pub Date : 2017-09-20 , DOI: 10.1016/j.jaci.2017.08.020 Julia A Wisniewski 1 , Lyndsey M Muehling 2 , Jacob D Eccles 2 , Brian J Capaldo 3 , Rachana Agrawal 2 , Debbie-Ann Shirley 4 , James T Patrie 5 , Lisa J Workman 2 , Alexander J Schuyler 2 , Monica G Lawrence 2 , W Gerald Teague 4 , Judith A Woodfolk 2
Journal of Allergy and Clinical Immunology ( IF 14.2 ) Pub Date : 2017-09-20 , DOI: 10.1016/j.jaci.2017.08.020 Julia A Wisniewski 1 , Lyndsey M Muehling 2 , Jacob D Eccles 2 , Brian J Capaldo 3 , Rachana Agrawal 2 , Debbie-Ann Shirley 4 , James T Patrie 5 , Lisa J Workman 2 , Alexander J Schuyler 2 , Monica G Lawrence 2 , W Gerald Teague 4 , Judith A Woodfolk 2
Affiliation
|
BACKGROUND
The pathogenesis of severe asthma in childhood remains poorly understood.
OBJECTIVE
We sought to construct the immunologic landscape in the airways of children with severe asthma.
METHODS
Comprehensive analysis of multiple cell types and mediators was performed by using flow cytometry and a multiplex assay with bronchoalveolar lavage (BAL) specimens (n = 68) from 52 highly characterized allergic and nonallergic children (0.5-17 years) with severe treatment-refractory asthma. Multiple relationships were tested by using linear mixed-effects modeling.
RESULTS
Memory CCR5+ TH1 cells were enriched in BAL fluid versus blood, and pathogenic respiratory viruses and bacteria were readily detected. IFN-γ+IL-17+ and IFN-γ-IL-17+ subsets constituted secondary TH types, and BAL fluid CD8+ T cells were almost exclusively IFN-γ+. The TH17-associated mediators IL-23 and macrophage inflammatory protein 3α/CCL20 were highly expressed. Despite low TH2 numbers, TH2 cytokines were detected, and TH2 skewing correlated with total IgE levels. Type 2 innate lymphoid cells and basophils were scarce in BAL fluid. Levels of IL-5, IL-33, and IL-28A/IFN-λ2 were increased in multisensitized children and correlated with IgE levels to dust mite, ryegrass, and fungi but not cat, ragweed, or food sources. Additionally, levels of IL-5, but no other cytokine, increased with age and correlated with eosinophil numbers in BAL fluid and blood. Both plasmacytoid and IgE+FcεRI+ myeloid dendritic cells were present in BAL fluid.
CONCLUSIONS
The lower airways of children with severe asthma display a dominant TH1 signature and atypical cytokine profiles that link to allergic status. Our findings deviate from established paradigms and warrant further assessment of the pathogenicity of TH1 cells in patients with severe asthma.
中文翻译:

无论过敏状态如何,重度哮喘患儿的下呼吸道均存在TH1信号。
背景技术关于儿童严重哮喘的发病机理仍然知之甚少。目的我们试图建立重症哮喘儿童气道的免疫学格局。方法采用流式细胞仪和多重分析法对52例具有严重治疗难治性的高度过敏和非过敏性儿童(0.5-17岁)的支气管肺泡灌洗(BAL)标本(n = 68)进行了多种细胞类型和介质的综合分析。哮喘。通过使用线性混合效应模型测试了多个关系。结果记忆CCR5 + TH1细胞相对于血液富含BAL液,并且容易检测到病原性呼吸道病毒和细菌。IFN-γ+ IL-17 +和IFN-γ-IL-17+子集构成继发性TH类型,而BAL液CD8 + T细胞几乎完全是IFN-γ+。与TH17相关的介质IL-23和巨噬细胞炎性蛋白3α/ CCL20高表达。尽管TH2值低,但仍检测到TH2细胞因子,并且TH2的偏斜与总IgE水平相关。BAL液中缺乏2型先天性淋巴样细胞和嗜碱性粒细胞。多敏感儿童的IL-5,IL-33和IL-28A /IFN-λ2水平升高,并且与尘螨,黑麦草和真菌的IgE水平相关,但与猫,豚草或食物来源无关。此外,IL-5的水平(但没有其他细胞因子)随着年龄增长而增加,并且与BAL液和血液中的嗜酸性粒细胞数量相关。BAL液中同时存在浆细胞样和IgE +FcεRI+髓样树突状细胞。结论患有严重哮喘的儿童的下呼吸道显示出主要的TH1信号和非典型的细胞因子,与过敏状态有关。
更新日期:2017-09-20
中文翻译:

无论过敏状态如何,重度哮喘患儿的下呼吸道均存在TH1信号。
背景技术关于儿童严重哮喘的发病机理仍然知之甚少。目的我们试图建立重症哮喘儿童气道的免疫学格局。方法采用流式细胞仪和多重分析法对52例具有严重治疗难治性的高度过敏和非过敏性儿童(0.5-17岁)的支气管肺泡灌洗(BAL)标本(n = 68)进行了多种细胞类型和介质的综合分析。哮喘。通过使用线性混合效应模型测试了多个关系。结果记忆CCR5 + TH1细胞相对于血液富含BAL液,并且容易检测到病原性呼吸道病毒和细菌。IFN-γ+ IL-17 +和IFN-γ-IL-17+子集构成继发性TH类型,而BAL液CD8 + T细胞几乎完全是IFN-γ+。与TH17相关的介质IL-23和巨噬细胞炎性蛋白3α/ CCL20高表达。尽管TH2值低,但仍检测到TH2细胞因子,并且TH2的偏斜与总IgE水平相关。BAL液中缺乏2型先天性淋巴样细胞和嗜碱性粒细胞。多敏感儿童的IL-5,IL-33和IL-28A /IFN-λ2水平升高,并且与尘螨,黑麦草和真菌的IgE水平相关,但与猫,豚草或食物来源无关。此外,IL-5的水平(但没有其他细胞因子)随着年龄增长而增加,并且与BAL液和血液中的嗜酸性粒细胞数量相关。BAL液中同时存在浆细胞样和IgE +FcεRI+髓样树突状细胞。结论患有严重哮喘的儿童的下呼吸道显示出主要的TH1信号和非典型的细胞因子,与过敏状态有关。



























 京公网安备 11010802027423号
京公网安备 11010802027423号