JAMA Oncology ( IF 28.4 ) Pub Date : 2017-09-01 , DOI: 10.1001/jamaoncol.2017.0368 Deena R Levine 1 , Belinda N Mandrell 2 , April Sykes 3 , Michele Pritchard 2 , Deborah Gibson 1 , Heather J Symons 4 , David Wendler 5 , Justin N Baker 1
|
Importance Early palliative care integration for cancer patients is now touted as the optimal care model, yet significant barriers often prevent its implementation. A perceived barrier, especially for pediatric oncology patients, is the notion that patients and their families may not need or want palliative care involvement early in the disease trajectory.
Objective To determine the perception of symptom burden early in treatment and assess attitudes toward early integration of palliative care in pediatric oncology patient-parent pairs.
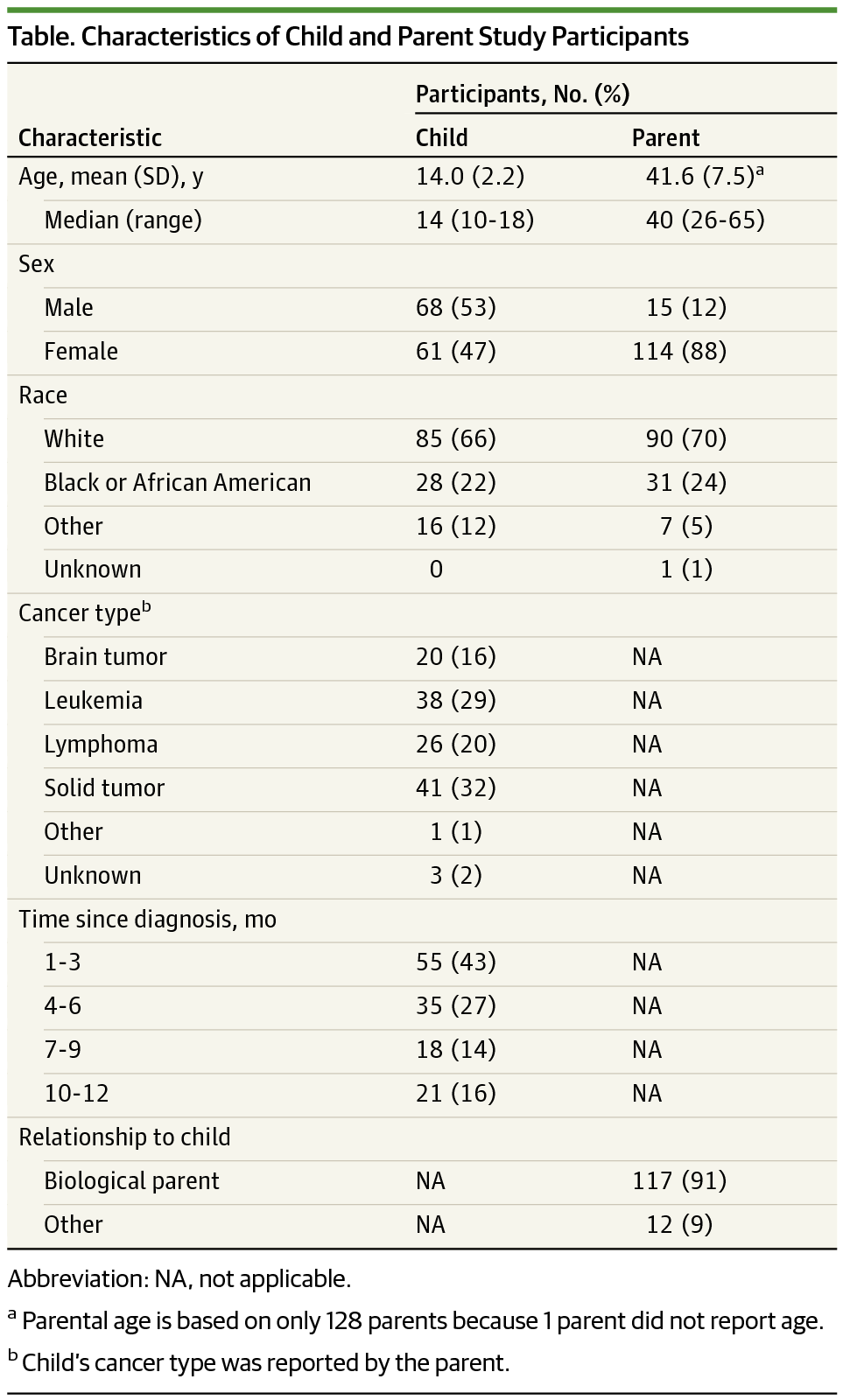
Design, Setting, and Participants Novel but pretested survey tools were administered to 129 patient-parent dyads of hospital-based pediatric oncology ambulatory clinics and inpatient units between September 2011 and January 2015. All patient participants were aged between 10 and 17 years and were diagnosed as having an oncologic condition 1 month to 1 year before enrollment. Both the patient and the parent in the dyad spoke English, and all participating parents provided written informed consent. A convenience sample was used for selection, with participants screened when otherwise presenting at a participating site. A total of 280 eligible participants were approached for study inclusion, 258 of whom were enrolled in the study (92.1% positive response-rate).
Main Outcomes and Measures Degree of perceived suffering from early symptom-related causes, attitudes toward early palliative care integration, and patient-parent concordance. Statistical analysis included descriptive statistics, calculation of concordance, McNemar test results, and Cochran-Armitage trend test results.
Results Of the 129 patients in the dyads, 68 were boys, and 61 girls; of the 129 parents, 15 were men, and 114 women. Patients reported the following symptoms in the first month of cancer therapy: nausea (n = 109; 84.5%), loss of appetite (n = 97; 75.2%), pain (n = 96; 74.4%), anxiety (n = 77; 59.7%), constipation (n = 69; 53.5%), depression (n = 64; 49.6%), and diarrhea (n = 52; 40.3%). A large proportion of those reporting suffering indicated substantial suffering severity from specific symptoms (ie, a great deal or a lot) including nausea, 52.3% (57 of 109), loss of appetite, 50.5% (49 of 97), constipation 30.4% (21 of 69), pain 30.2% (29 of 96), anxiety 28.6% (22 of 77), depression 28.1% (18 of 64), and diarrhea 23.1% (12 of 52). Few children and parents expressed opposition to early palliative care involvement (2 [1.6%] and 8 [6.2%]) or perceived any detrimental effects on their relationship with their oncologist (6 [4.7%] and 5 [3.9%]), loss of hope (3 [2.3%] and 10 [7.8%]), or therapy interference (3 [2.3%] and 2 [1.6%], respectively). Intradyad concordance was low overall: 26% to 29% for exact concordance and 40% to 69% for agreement within 1 response category. Significant differences in patient-parent attitudes toward aspects of early palliative care included child participants being more likely than their parents (40.3% [n = 52] vs 17.8% [n = 23]) to indicate that palliative care would have been helpful for treating their symptoms (P < .001).
Conclusions and Relevance Pediatric oncology patients experience a high degree of symptom-related suffering early in cancer therapy, and very few patients or parents in this study expressed negative attitudes toward early palliative care. Our findings suggest that pediatric oncology patients and families might benefit from, and are not a barrier to, early palliative care integration in oncology.
中文翻译:

患者和父母对儿科肿瘤学早期姑息治疗整合的需求、态度和看法
重要性 癌症患者的早期姑息治疗整合现在被吹捧为最佳护理模式,但重大障碍往往阻碍其实施。一个明显的障碍,特别是对于儿科肿瘤患者来说,是患者及其家人可能不需要或不希望在疾病轨迹早期参与姑息治疗的概念。
目的 确定治疗早期对症状负担的感知,并评估儿童肿瘤患者父母对早期整合姑息治疗的态度。
设计、设置和参与者 2011 年 9 月至 2015 年 1 月期间,对医院儿科肿瘤门诊和住院病房的 129 名患者父母进行了新的但经过预先测试的调查工具。所有患者参与者的年龄在 10 至 17 岁之间,并被诊断出入组前 1 个月至 1 年患有肿瘤疾病。二人组中的患者和父母都说英语,所有参与的父母都提供了书面知情同意书。一个方便的样本被用于选择,当参与者以其他方式出现在参与站点时进行筛选。共有 280 名符合条件的参与者被纳入研究,其中 258 人参加了研究(阳性反应率为 92.1%)。
主要结果和措施 对早期症状相关原因的感知痛苦程度、对早期姑息治疗整合的态度以及患者与父母的一致性。统计分析包括描述性统计、一致性计算、McNemar 检验结果和 Cochran-Armitage 趋势检验结果。
结果 129 名患者中,男孩 68 人,女孩 61 人;在 129 位父母中,15 位是男性,114 位是女性。患者在癌症治疗的第一个月报告了以下症状:恶心(n = 109;84.5%)、食欲不振(n = 97;75.2%)、疼痛(n = 96;74.4%)、焦虑(n = 77 ; 59.7%)、便秘 (n = 69; 53.5%)、抑郁症 (n = 64; 49.6%) 和腹泻 (n = 52; 40.3%)。大部分报告遭受痛苦的人表示严重遭受特定症状(即很多或很多)包括恶心,52.3%(109 人中的 57 人),食欲不振,50.5%(97 人中的 49 人),便秘 30.4% (21 of 69)、疼痛 30.2% (29 of 96)、焦虑 28.6% (22 of 77)、抑郁 28.1% (18 of 64) 和腹泻 23.1% (12 of 52)。很少有儿童和父母反对早期姑息治疗参与(2 [1.6%] 和 8 [6. 2%])或认为对他们与肿瘤科医生的关系有任何不利影响(6 [4.7%] 和 5 [3.9%])、失去希望(3 [2.3%] 和 10 [7.8%])或治疗干扰( 3 [2.3%] 和 2 [1.6%],分别)。Intradyad 的一致性总体较低:精确一致性为 26% 至 29%,1 个响应类别内的一致性为 40% 至 69%。患者与父母对早期姑息治疗的态度存在显着差异,包括儿童参与者比他们的父母(40.3% [n = 52] vs 17.8% [n = 23])更有可能表明姑息治疗有助于治疗他们的症状(26% 到 29% 表示完全一致,40% 到 69% 表示在 1 个响应类别内一致。患者与父母对早期姑息治疗的态度存在显着差异,包括儿童参与者比他们的父母(40.3% [n = 52] vs 17.8% [n = 23])更有可能表明姑息治疗有助于治疗他们的症状(26% 到 29% 表示完全一致,40% 到 69% 表示在 1 个响应类别内一致。患者与父母对早期姑息治疗的态度存在显着差异,包括儿童参与者比他们的父母(40.3% [n = 52] vs 17.8% [n = 23])更有可能表明姑息治疗有助于治疗他们的症状(P < .001)。
结论和相关性 儿科肿瘤患者在癌症治疗早期会经历高度的症状相关痛苦,本研究中很少有患者或父母对早期姑息治疗表示消极态度。我们的研究结果表明,儿科肿瘤患者和家属可能会受益于肿瘤学中的早期姑息治疗整合,而不是障碍。

























 京公网安备 11010802027423号
京公网安备 11010802027423号