当前位置:
X-MOL 学术
›
J. Hepatol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Cytotherapy with M1-polarized macrophages ameliorates liver fibrosis by modulating immune microenvironment in mice
Journal of Hepatology ( IF 25.7 ) Pub Date : 2017-10-01 , DOI: 10.1016/j.jhep.2017.05.022 Peng-Fei Ma , Chun-Chen Gao , Jing Yi , Jun-Long Zhao , Shi-Qian Liang , Yang Zhao , Yu-Chen Ye , Jian Bai , Qi-Jun Zheng , Ke-Feng Dou , Hua Han , Hong-Yan Qin
Journal of Hepatology ( IF 25.7 ) Pub Date : 2017-10-01 , DOI: 10.1016/j.jhep.2017.05.022 Peng-Fei Ma , Chun-Chen Gao , Jing Yi , Jun-Long Zhao , Shi-Qian Liang , Yang Zhao , Yu-Chen Ye , Jian Bai , Qi-Jun Zheng , Ke-Feng Dou , Hua Han , Hong-Yan Qin
|
BACKGROUND & AIMS
Macrophages play vital roles in chronic liver injury, and have been tested as a tool for cytotherapy in liver fibrosis. However, macrophages possess ontogenic and functional heterogeneities. Some subsets are pro-fibrotic, whereas others are anti-fibrotic. This study aimed to clarify which macrophage subset is efficient for cytotherapy in liver fibrosis and to elucidate the underlying mechanisms. METHODS
Liver fibrosis was induced in mice by carbon tetrachloride injection or bile duct ligation. Bone-marrow-derived macrophages (BMDMs) were polarized into M0, M1, or M2 macrophages, respectively. BMDMs were infused into mice through the tail vein at different stages of fibrogenesis. Fibrosis progression, hepatic cell populations, and related molecular changes were evaluated. RESULTS
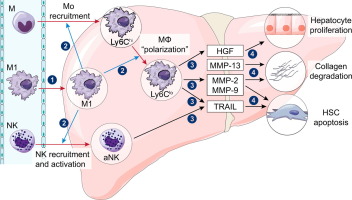
Both M0 and M1 BMDMs significantly ameliorated liver fibrosis, but M1 exhibited stronger therapeutic effects than M0. M2 macrophages were not effective on liver fibrosis. M1 macrophages reduced the number and activation of hepatic stellate cells (HSCs), which could be attributed at least partly to increased HSC apoptosis. M1 macrophages enhanced the recruitment of endogenous macrophages into fibrotic liver, which displayed the phenotype of Ly6Clo restorative macrophages and produced matrix metalloproteinases (MMPs) and hepatic growth factor (HGF) to enhance collagen degradation and hepatocyte proliferation, respectively. M1 macrophages also increased the number of total and activated natural killer (NK) cells in the fibrotic liver, which released TNF-related apoptosis-inducing ligand (TRAIL), inducing HSC apoptosis. CONCLUSIONS
M1 macrophages, which modulate the immune microenvironment to recruit and modify the activation of endogenous macrophages and NK cells, are effective for cytotherapy in experimental liver fibrosis. Lay summary: M1 Bone marrow-derived macrophages (BMDMs) exhibit a stronger therapeutic effect by modulating the hepatic microenvironment to recruit and modify the activation of endogenous macrophages and natural killer (NK) cells, which likely lead to hepatic stellate cells (HSCs) apoptosis and hampered fibrogenesis.
中文翻译:

M1极化巨噬细胞细胞疗法通过调节小鼠免疫微环境改善肝纤维化
背景和目的 巨噬细胞在慢性肝损伤中起着至关重要的作用,并且已被测试作为肝纤维化细胞治疗的工具。然而,巨噬细胞具有个体发生和功能异质性。一些亚群是促纤维化的,而其他亚群是抗纤维化的。本研究旨在阐明哪种巨噬细胞亚群对肝纤维化的细胞治疗有效,并阐明其潜在机制。方法四氯化碳注射液或胆管结扎法诱导小鼠肝纤维化。骨髓来源的巨噬细胞 (BMDM) 分别极化为 M0、M1 或 M2 巨噬细胞。BMDMs 在纤维化的不同阶段通过尾静脉注入小鼠体内。评估了纤维化进展、肝细胞群和相关的分子变化。结果 M0 和 M1 BMDMs 均显着改善肝纤维化,但 M1 表现出比 M0 更强的治疗效果。M2巨噬细胞对肝纤维化无效。M1 巨噬细胞减少了肝星状细胞 (HSC) 的数量和活化,这至少部分归因于 HSC 凋亡增加。M1 巨噬细胞增强内源性巨噬细胞向纤维化肝脏的募集,显示出 Ly6Clo 修复性巨噬细胞的表型,并产生基质金属蛋白酶 (MMP) 和肝生长因子 (HGF),分别增强胶原降解和肝细胞增殖。M1 巨噬细胞还增加了纤维化肝脏中总和活化的自然杀伤 (NK) 细胞的数量,从而释放了 TNF 相关的凋亡诱导配体 (TRAIL),诱导 HSC 凋亡。结论 M1 巨噬细胞调节免疫微环境以募集和改变内源性巨噬细胞和 NK 细胞的激活,对实验性肝纤维化的细胞治疗有效。总结:M1 骨髓源性巨噬细胞 (BMDMs) 通过调节肝脏微环境来招募和改变内源性巨噬细胞和自然杀伤 (NK) 细胞的活化,从而表现出更强的治疗效果,这可能导致肝星状细胞 (HSC) 凋亡并阻碍纤维化。
更新日期:2017-10-01
中文翻译:

M1极化巨噬细胞细胞疗法通过调节小鼠免疫微环境改善肝纤维化
背景和目的 巨噬细胞在慢性肝损伤中起着至关重要的作用,并且已被测试作为肝纤维化细胞治疗的工具。然而,巨噬细胞具有个体发生和功能异质性。一些亚群是促纤维化的,而其他亚群是抗纤维化的。本研究旨在阐明哪种巨噬细胞亚群对肝纤维化的细胞治疗有效,并阐明其潜在机制。方法四氯化碳注射液或胆管结扎法诱导小鼠肝纤维化。骨髓来源的巨噬细胞 (BMDM) 分别极化为 M0、M1 或 M2 巨噬细胞。BMDMs 在纤维化的不同阶段通过尾静脉注入小鼠体内。评估了纤维化进展、肝细胞群和相关的分子变化。结果 M0 和 M1 BMDMs 均显着改善肝纤维化,但 M1 表现出比 M0 更强的治疗效果。M2巨噬细胞对肝纤维化无效。M1 巨噬细胞减少了肝星状细胞 (HSC) 的数量和活化,这至少部分归因于 HSC 凋亡增加。M1 巨噬细胞增强内源性巨噬细胞向纤维化肝脏的募集,显示出 Ly6Clo 修复性巨噬细胞的表型,并产生基质金属蛋白酶 (MMP) 和肝生长因子 (HGF),分别增强胶原降解和肝细胞增殖。M1 巨噬细胞还增加了纤维化肝脏中总和活化的自然杀伤 (NK) 细胞的数量,从而释放了 TNF 相关的凋亡诱导配体 (TRAIL),诱导 HSC 凋亡。结论 M1 巨噬细胞调节免疫微环境以募集和改变内源性巨噬细胞和 NK 细胞的激活,对实验性肝纤维化的细胞治疗有效。总结:M1 骨髓源性巨噬细胞 (BMDMs) 通过调节肝脏微环境来招募和改变内源性巨噬细胞和自然杀伤 (NK) 细胞的活化,从而表现出更强的治疗效果,这可能导致肝星状细胞 (HSC) 凋亡并阻碍纤维化。



























 京公网安备 11010802027423号
京公网安备 11010802027423号